Chapter: Medical Surgical Nursing: Emergency Nursing
Heat Stroke - Environmental Emergencies
Environmental
Emergencies
HEAT STROKE
Heat stroke is an acute
medical emergency caused by failure of the heat-regulating mechanisms of the
body. It usually occurs during extended heat waves, especially when they are
accompanied by high humidity. People at risk are those not acclimatized to
heat, elderly and very young people, those unable to care for them-selves,
those with chronic and debilitating diseases, and those taking certain
medications (eg, major tranquilizers, anticholiner-gics, diuretics,
beta-adrenergic blocking agents). Exertional heat stroke occurs in healthy
individuals during sports or work activ-ities (eg, exercising in extreme heat
and humidity). Hyperthermiaresults because of inadequate
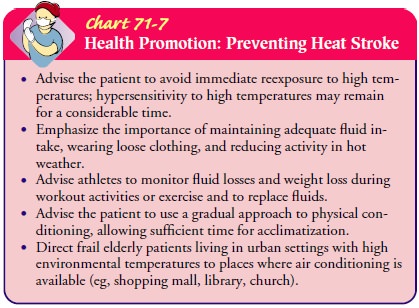
heat loss. This type of heat stroke can also cause death. See Chart 71-7 for
prevention strategies.
Gerontologic Considerations
Most heat-related deaths
occur in the elderly, because their cir-culatory systems are unable to
compensate for stress imposed by heat. Elderly people have a decreased ability
to perspire as well as a decreased thirst mechanism to compensate for heat.
Assessment and Diagnostic Findings
Heat stroke causes thermal injury at the cellular level,
resulting in widespread damage to the heart, liver, kidney, and blood
coagu-lation. Recent patient history reveals exposure to elevated ambient
temperature or excessive exercise during extreme heat. When as-sessing the
patient, the nurse notes the following symptoms: profound central nervous
system (CNS) dysfunction (manifested by confusion, delirium, bizarre behavior,
coma); elevated body temperature (40.6°C [105°F] or higher); hot, dry skin;
and usually anhidrosis (absence of sweating), tachypnea, hypotension, and
tachycardia.
Management
The primary goal is to reduce the high temperature as
quickly as possible, because mortality is directly related to the duration of
hyperthermia. Simultaneous treatment focuses on stabilizing oxy-genation using
the ABCs of basic life support.
After the patient’s clothing is removed, the core
(internal) temperature is reduced to 39°C (102°F) as rapidly as possible. One
or more of the following methods may be used as directed:
·
Cool sheets and towels or
continuous sponging with cool water
·
Ice applied to the neck,
groin, chest, and axillae while spray-ing with tepid water
·
Cooling blankets
·
Iced saline lavage of the
stomach or colon if the temperature does not decrease
·
Immersion of the patient in a
cold water bath (if possible)
During cooling, the patient is massaged to promote circulation and maintain cutaneous vasodilation. An electric fan is positioned so that it blows on the patient to augment heat dissipation by convection and evaporation. The patient’s temperature is constantly monitored with a thermistor placed in the rectum, bladder, or esophagus to evaluate core temperature. Caution is used to avoid hypothermia and to prevent hyperthermia, which may recur spontaneously within 3 to 4 hours.
Throughout treatment,
the patient’s status is monitored care-fully, including vital signs, ECG
findings (for possible myo-cardial ischemia, myocardial infarction, and
dysrhythmias), CVP, and level of responsiveness, all of which may change with
rapid alterations in body temperature. A seizure may be followed by re-currence
of hyperthermia. To meet tissue needs exaggerated by the hypermetabolic
condition, 100% oxygen is administered. The patient may require endotracheal
intubation and mechanical ven-tilation to support failing cardiopulmonary
systems.
Intravenous infusion therapy of normal saline or lactated
Ringer’s solution is initiated as directed to replace fluid losses and maintain
adequate circulation. Fluids are administered carefully because of the dangers
of myocardial injury from high body tem-perature and poor renal function.
Cooling redistributes fluid volume from the periphery to the core.
Urine output is also
measured frequently, because acute tubu-lar necrosis is a complication of heat
stroke from rhabdomyolysis (myoglobin in the urine). Blood specimens are
obtained for ser-ial testing to detect bleeding disorders, such as disseminated
intra-vascular coagulopathy, and for serial enzyme studies to estimate thermal
hypoxic injury to the liver, heart, and muscle tissue. Permanent liver,
cardiac, and CNS damage may occur.
Additional supportive care may include dialysis for renal
fail-ure, antiseizure agents to control seizures, potassium for hypo-kalemia,
and sodium bicarbonate to correct metabolic acidosis. Benzodiazepines or
chlorpromazine may be prescribed to sup-press seizure activity. Patient education
regarding the prevention of heat stroke (ie, adequate fluid intake, staying out
of the sun es-pecially between 10 AM and 2 PM) is also important to
prevent a recurrence of heat stroke.
Related Topics