Chapter: Medical Surgical Nursing: Emergency Nursing
Hemorrhage - Emergency Nursing
Hemorrhage
Only a few conditions, such as obstructed airway or a sucking wound of the chest, take precedence over the immediate control of hemorrhage. Stopping bleeding is essential to the care and sur-vival of patients in an emergency or disaster situation. Hemor-rhage that results in the reduction of circulating blood volume is a primary cause of shock. Minor bleeding, which is usually venous, generally stops spontaneously unless the patient has a bleeding disorder or has been taking anticoagulants.
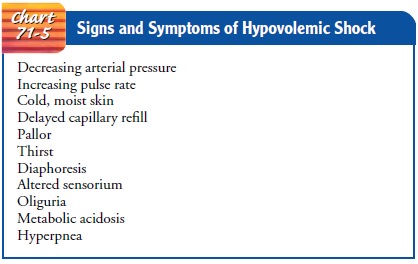
The patient is assessed
for signs and symptoms of shock: cool, moist skin (resulting from poor
peripheral perfusion), falling blood pressure, increasing heart rate, delayed
capillary refill, and decreasing urine volume (a late sign) (Chart 71-5). The
goals of emergency management are to control the bleeding, maintain an
adequately circulating blood volume for tissue oxygenation, and prevent shock.
Patients who hemorrhage are at risk for cardiac ar-rest caused by hypovolemia
with secondary anoxia. Nursing in-terventions are carried out collaboratively
with other members of the emergency health care team.
Management
FLUID REPLACEMENT
Whenever a patient is experiencing hemorrhage—whether exter-nal or internal—a loss of circulating blood results in a fluid vol-ume deficit and decreased cardiac output. Therefore, fluid replacement is imperative to maintain circulation. Typically, two large-bore intravenous cannulae are inserted to provide a means for fluid and blood replacement, and blood samples are obtained for analysis, typing, and cross-matching.
Replacement fluids are administered as prescribed, depending on clinical
estimates of the type and volume of fluid lost. Replacement fluids may include
isotonic electrolyte solutions (lactated Ringer’s, normal saline), colloid, and
blood component therapy.
Packed red blood cells are infused when there is massive
blood loss. In emergencies, O-negative blood is used for women of childbearing
age and O-positive blood is used for men and for postmenopausal women. In an
emergent situation, there is not time to type and cross-match or type and
screen blood. O-negative blood provides safe administration of blood imme-diately
without sensitizing an Rh-negative woman to Rh-positive blood. Sensitization
can result in difficulties during pregnancy later.
Additional platelets and clotting factors are given when large amounts of blood are needed, because replacement blood is defi-cient in clotting factors
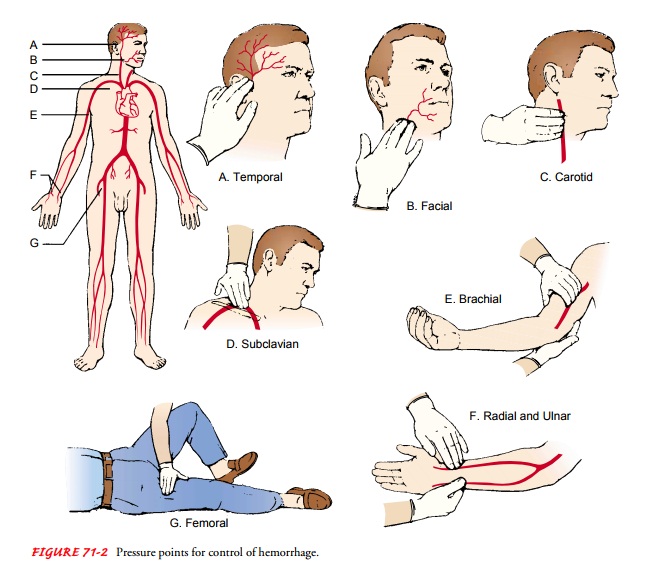
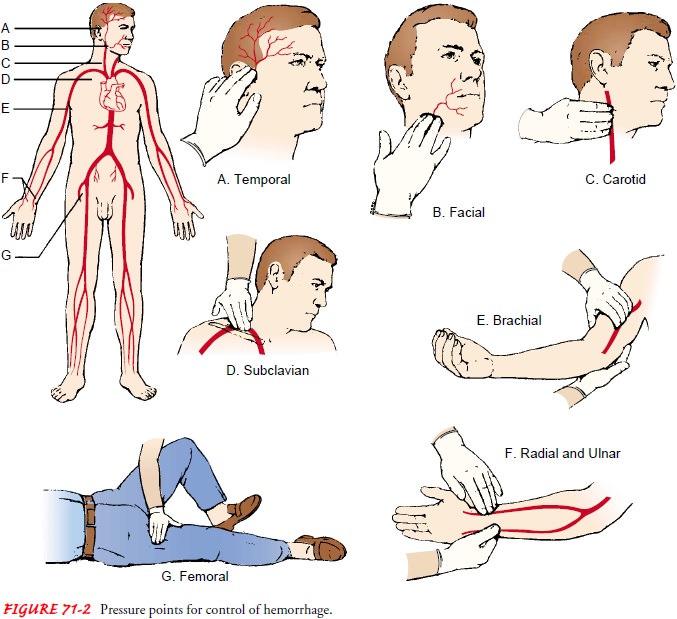
CONTROL OF EXTERNAL HEMORRHAGE
If a patient is
hemorrhaging externally (eg, from a wound), a rapid physical assessment is
performed as the patient’s clothing is cut away in an attempt to identify the
area of hemorrhage. Direct, firm pressure is applied over the bleeding area or
the involved artery (Fig. 71-2). Most bleeding can be stopped or at least
controlled by application of direct pressure. Otherwise, unchecked arterial
bleeding results in death. A firm pressure dressing is applied, and the injured
part is elevated to stop venous and capillary bleeding if possible. If the
injured area is an ex-tremity, the extremity is immobilized to control blood
loss.
Tourniquets.
A tourniquet is applied to an extremity only as alast resort when the external hemorrhage cannot be controlled inany
other way. Care must be taken when applying a tourniquet because of the risk of
loss of the extremity. The tourniquet is ap-plied just proximal to the wound
and tied tightly enough to con-trol arterial blood flow. The patient is tagged
with a skin-marking pencil or on adhesive tape on the forehead with a “T,”
stating the location of the tourniquet and the time applied. Periodically, the
tourniquet is loosened to prevent irreparable vascular or neuro-logic damage.
If there is arterial bleeding, the tourniquet is re-moved and a pressure
dressing is applied. If the patient has suffered a traumatic amputation with
uncontrollable hemorrhage, the tourniquet remains in place until the patient is
in the operat-ing room.
CONTROL OF INTERNAL BLEEDING
If the patient shows no external signs of bleeding but exhibits tachycardia, falling blood pressure, thirst, apprehension, cool and moist skin, or delayed capillary refill, internal hemorrhage is sus-pected.
Typically, packed red blood cells (O-negative) are
ad-ministered at a rapid rate, and the patient is prepared for more definitive
treatment (eg, surgery, pharmacologic therapy). Addi-tionally, arterial blood
specimens are obtained to evaluate pul-monary function and tissue perfusion and
to establish baseline hemodynamic parameters, which are then used as an index
for determining the amount of fluid replacement the patient can tol-erate and
the response to therapy. The patient is maintained in the supine position and
monitored closely until hemodynamic or circulatory parameters improve, or until
transport to the operating room or intensive care.
Related Topics