Chapter: Medical Surgical Nursing: Emergency Nursing
Scope and Practice of Emergency Nursing
Scope and
Practice of Emergency Nursing
The emergency nurse has
had specialized education, training, and experience to gain expertise in
assessing and identifying patients’ health care problems in crisis situations.
In addition, the emer-gency nurse establishes priorities, monitors and
continuously as-sesses acutely ill and injured patients, supports and attends
to families, supervises allied health personnel, and teaches patients and
families within a time-limited, high-pressured care environ-ment. Nursing
interventions are accomplished interdependently, in consultation with or under
the direction of a licensed physi-cian or nurse practitioner. The strengths of
nursing and medicine are complementary in an emergency situation. Appropriate
nurs-ing and medical interventions are anticipated based on assess-ment data.
The emergency health care staff members work as a team in performing the highly
technical, hands-on skills required to care for patients in an emergency
situation.
The nursing process provides a
logical framework for problem solving in this environment. Patients in the ED
have a wide variety of actual or potential problems, and their condition may
change constantly. Therefore, nursing assessment must be continuous, and
nursing diagnoses change with the patient’s condition. Although a patient may
have several diagnoses at a given time, the focus is on the most
life-threatening ones; often, both independent and interdependent nursing
interventions are required.
ISSUES IN EMERGENCY NURSING CARE
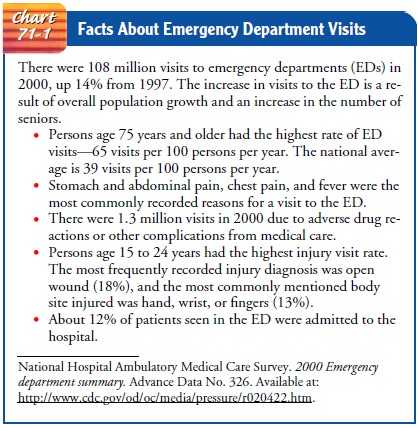
Emergency nursing is
demanding because of the diversity of con-ditions and situations that, if not
unique to the ED, certainly pre-sent a challenge (Chart 71-1). These issues
include legal issues, occupational health and safety risks for ED staff, and
the chal-lenge of providing holistic care in the context of a fast-paced,
technology-driven environment in which serious illness and death are confronted
on a daily basis. Another dimension of emergency nursing is nursing in
disasters. With the increasing use of weapons of terror and mass destruction,
the emergency nurse must expand his or her knowledge base to encompass
recognizing and treating patients exposed to biologic and other terror weapons
and anticipate nursing care in the event of a mass casualty inci-dent.
Documentation of Consent
Consent to examine and
treat the patient is part of the ED record. The patient must consent to
invasive procedures (eg, angiogra-phy, lumbar puncture) unless he or she is
unconscious or in crit-ical condition and unable to make decisions. If the
patient is unconscious and brought to the ED without family or friends, this
fact should be documented. Monitoring of the patient’s con-dition, as well as
all instituted treatments and the times at which they were performed, must be
documented. After treatment, a notation is made on the record about the
patient’s condition on discharge or transfer and about instructions given to
the patient and family for follow-up care.
Limiting Exposure to Health Risks
Because of the
increasing numbers of people infected with hep-atitis B and with human
immunodeficiency virus (HIV), health care providers are at an increased risk
for exposure to communi-cable diseases through blood or other body fluids. This
risk is fur-ther compounded in the ED because of the common use of invasive
treatments in addition to the wide range of patient con-ditions. All emergency
health care providers should adhere strictly to standard precautions for
minimizing exposure.
The reemergence of tuberculosis, a major health problem, is complicated by multidrug-resistant tuberculosis and by tubercu-losis concomitant with HIV infection. Early identification and adherence to transmission-based precautions for patients who are potentially infectious is crucial. Nurses in the ED are usually fitted with a personal high-efficiency particulate air (HEPA)-filter mask apparatus to use when treating patients with airborne diseases.
The potential for exposure to highly contagious
organisms, hazardous chemicals or gases, and radiation related to acts of
ter-rorism or natural or manmade disasters present additional risks to ED
staff.
Providing Holistic Care
Sudden illness or trauma
is a stress to physiologic and psycho-logical homeostasis that requires
physiologic and psychological healing. Patients and families experiencing
sudden injury or ill-ness often are overwhelmed by anxiety because they have
not had time to adapt to the crisis. They experience real and terrifying fear
of death, mutilation, immobilization, and other assaults on their personal
identity and body integrity. When confronted with trauma, severe disfigurement,
severe illness, or sudden death, the family experiences several stages of
crisis. The stages begin with anxiety and progress through denial, remorse and
guilt, anger, grief, and reconciliation. The initial goal for the patient and
family is anxiety reduction, a prerequisite to recovering the ability to cope.
Assessment of the patient and family’s psychological
function includes evaluating emotional expression, degree of anxiety, and
cognitive functioning. Possible nursing diagnoses include anxiety related to
uncertain potential outcomes of the illness or trauma and ineffective
individual coping related to acute situational crisis. In addition to anxiety,
possible nursing diagnoses for the family include anticipatory grieving and
alterations in family processes related to acute situational crises.
PATIENT-FOCUSED INTERVENTIONS
Those caring for the
patient should act confidently and compe-tently to relieve anxiety. Reacting
and responding to the patient in a warm manner promotes a sense of security.
Explanations should be given on a level that the patient can understand,
because an informed patient is better able to cope positively with stress.
Human contact and reassuring words reduce the panic of the se-verely injured
person and aid in dispelling fear of the unknown.
The unconscious patient
should be treated as if conscious. That is, the patient should be touched,
called by name, and given an ex-planation of every procedure that is performed.
As the patient re-gains consciousness, the nurse should orient the patient by
stating his or her name, the date, and the location. This basic information
should be provided repeatedly, as needed, in a reassuring way.
FAMILY-FOCUSED INTERVENTIONS
The family is kept
informed about where the patient is, how he or she is doing, and the care that
is being given. Allowing the family to stay with the patient, when possible,
also helps allay their anx-ieties. Additional interventions are based on the
assessment of the stage of crisis that the family is experiencing. Measures to
help fam-ily members cope with sudden death are presented in Chart 71-2.
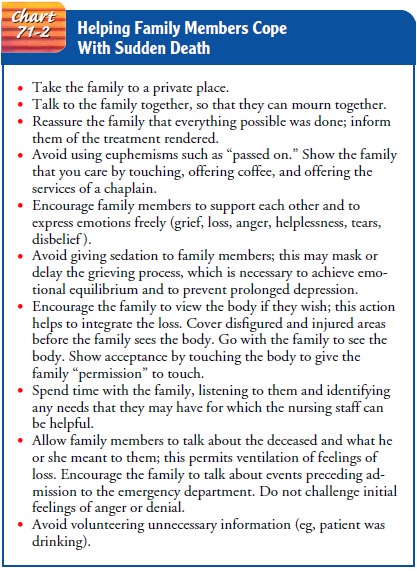
Anxiety
and Denial.During these stages,
family members are en-couraged to recognize and talk about their feelings of
anxiety. Asking questions is encouraged. Honest answers given at the level of
the family’s understanding must be provided. Although denial is an ego-defense
mechanism that protects one from recognizing painful and disturbing aspects of
reality, prolonged denial is not encouraged or supported. The family must be
prepared for the reality of what has happened and what may come.
Remorse and Guilt.Expressions of remorse and guilt may beheard, with family members accusing themselves (or each other) of negligence or minor omissions. Family members are urged to verbalize their feelings until they realize that there was probably little that they could have done to prevent the injury or illness.
Anger.Expressions of anger, common in crisis situations, are away of handling
anxiety and fear. Anger is frequently directed at the patient, but it is also
often expressed toward the physician, the nurse, or admitting personnel. The
therapeutic approach is to allow the anger to be ventilated, then assist the
family to identify their feelings of frustration.
Grief.Grief is a complex emotional response to
anticipated or ac-tual loss. The key nursing intervention is to help family
members work through their grief and to support their coping mecha-nisms,
letting them know that it is normal and acceptable for them to cry, feel pain,
and express loss. The hospital chaplain and social services staff both serve as
invaluable members of the team when assisting families to work through their
grief.
EMERGENCY NURSING AND THE CONTINUUM OF CARE
As stated previously,
one principle underlying emergency care is that the patient will be rapidly
assessed, treated, and referred to the appropriate setting for ongoing care.
This makes the ED a very temporary point on the continuum of care. Most
patients who receive emergency care are discharged directly from the ED to
their homes, and emergency nurses must plan and facilitate the patient’s safe
discharge and follow-up care in the home and the community.
Discharge Planning
Before discharge, instructions for continuing care are
given to the patient and the family or significant others. All instructions
should be given not only verbally but also in writing, so that the patient can
refer to them later. Many EDs have preprinted stan-dard instruction sheets for
the more common conditions. These instructions are then individualized for each
patient. These in-structions may be available in a variety of languages. If
they are not available in the language that the patient needs, an inter-preter
should be used. Instructions should include information about prescribed
medications, treatments, diet, activity, and when to contact a health care
provider or schedule follow-up appointments. It is imperative that instructions
are written leg-ibly, use simple language, and are clear in their teaching.
When providing discharge instructions, the nurse also considers any special
needs the patient may have related to hearing or visual deficits.
Community Services
Before discharge, some patients require the services of a
social worker to help them meet continuing health care needs. For pa-tients and
families who cannot provide care at home, community agencies (eg, Home Care
Nursing Services, Visiting Nurse Asso-ciation) may be contacted before
discharge to arrange services. This is particularly important for elderly
patients who need assis-tance. Identifying continuing health care needs and
making arrangements for meeting these needs can prevent return visits to the ED
and readmission to the hospital.
For patients who are
returning to extended care facilities and for those who already rely on
community agencies for continu-ing health care, communication about the
patient’s condition and any changes in health care needs that have occurred
must be provided to the appropriate facilities or agencies. This commu-nication
is essential to promote continuity of care and to ensure ongoing care to meet
the patient’s changing health care needs.
Gerontologic Considerations
The ED is a common point of entry into the health care
system for patients 65 years of age and older. In fact, patients in this age
group account for more than 99 million visits to emergency fa-cilities each
year (see Chart 71-1). Elderly patients typically arrive with one or more
presenting conditions involving the skin, cardio-vascular system, or abdomen.
Nonspecific symptoms, such as weakness and fatigue, episodes of falling,
incontinence, and change in mental status, may be manifestations of acute,
poten-tially life-threatening illness in the elderly person. Emergencies in
this age group may be more difficult to manage because elderly patients may
have
·
An atypical presentation
·
An altered response to
treatment
·
A greater risk of developing
complications
The elderly patient may perceive the emergency as a
crisis sig-naling the end of an independent lifestyle or even resulting in
death. The nurse should give attention to the patient’s feelings of anxiety and
fear.
The older patient may have fewer sources of social and
finan-cial support in addition to frail health. The nurse should assess the
psychosocial resources of the patient (and of the caregiver, if necessary) and
anticipate discharge needs. Referrals for support services (eg, to the social
service department or a gerontologic nurse specialist) may be necessary.
Related Topics