Chapter: Medical Surgical Nursing: Emergency Nursing
Anaphylactic Reaction - Environmental Emergencies
ANAPHYLACTIC REACTION
An anaphylactic reaction
is an acute systemic hypersensitivity re-action that occurs within seconds or
minutes after exposure to certain foreign substances, such as medications (eg,
penicillin, iodinated contrast material), and other agents, such as insectstings
(eg, bee, wasp, yellow jacket, hornet) or foods (eg, eggs, peanuts). Repeated
administration of parenteral or oral thera-peutic agents (eg, repeated
exposures to penicillin) may also pre-cipitate an anaphylactic reaction when
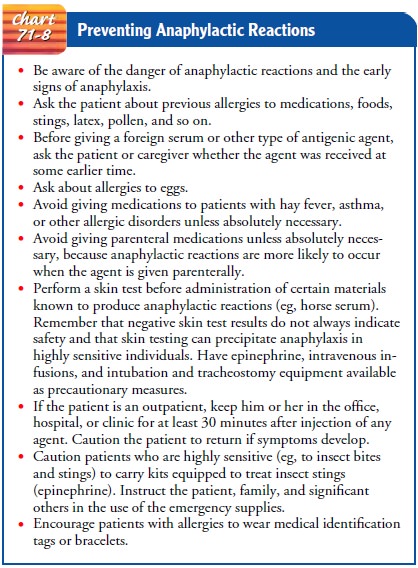
initially only a mild allergic response occurred. See Chart 71-8 for
anaphylaxis pre-vention strategies.
An anaphylactic reaction
is the result of an antigen–antibody interaction in a sensitized individual
who, as a consequence of previous exposure, has developed a special type of
antibody (immunoglobulin) that is specific for that particular allergen. The
antibody immunoglobulin E (IgE) is responsible for most of the immediate type
of human allergic responses. The individual be-comes sensitive to a particular
antigen after production of IgE to that antigen. A second exposure to the same
antigen results in a more severe and more rapid response.
Anaphylactic reaction produces a wide range of clinical
man-ifestations, especially respiratory symptoms (difficulty breathing and
stridor secondary to laryngeal edema), fainting, itching, swelling of mucous
membranes, and a sudden drop in blood pres-sure secondary to massive
vasodilation.
Management
With an anaphylactic reaction, establishing a patent airway and ventilation is essential. (This is performed while another person administers epinephrine.) Early endotracheal tube intubation is essential to avoid loss of the airway, and oropharyngeal suction may be necessary to remove excessive secretions. Resuscitative measures are used, especially for patients with stridor and pro-gressive pulmonary edema. If glottal edema occurs, a cricothy-roidotomy is used to provide an airway.
Simultaneously with airway management, aqueous
epineph-rine is administered as prescribed to provide rapid relief of the
hypersensitivity reaction. Epinephrine may be administered again, if necessary
and as prescribed. Judgment is used in choosing the route of administration, as
follows:
·
Subcutaneous injection for
mild, generalized symptoms
·
Intramuscular injection when
the reaction is more severe and progressive, and with concern that vascular
collapse will inhibit absorption
·
Intravenous route (aqueous epinephrine
diluted in saline solution and administered slowly),
used in rare instances in which there is complete loss of consciousness and
severe cardiovascular collapse. This method may precipitate car-diac
dysrhythmias. ECG monitoring with a readily avail-able defibrillator is
necessary. This method is controversial and is not usually recommended because
it can lead to more distress than is initially present. An intravenous infusion
of saline solution is initiated to provide for emergency access to a vein and
to treat hypotension.
Additional treatments may include
·
Antihistamines to block
further histamine binding at target cells
·
Aminophylline by slow
intravenous infusion for severe bronchospasm and wheezing refractory to other
treatment
·
Albuterol inhalers or
humidified treatments to decrease bronchoconstriction; crystalloids, colloids,
or vasopressors to treat prolonged hypotension
·
Isoproterenol or dopamine for
reduced cardiac output; oxy-gen to enhance tissue perfusion
·
Intravenous benzodiazepines
for control of seizures, and corticosteroids for prolonged reaction with
persistent hy-potension or bronchospasm
After the acute symptoms
have been treated, the patient is usu-ally admitted to the hospital for
observation. The patient should be informed about ways to prevent anaphylactic
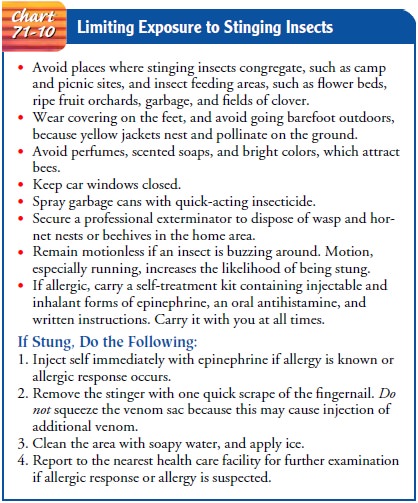
reactions. See Chart 71-10 for strategies to limit exposure to stinging
insects.
Related Topics