Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Wound Coverage: Grafts and Flaps
WOUND COVERAGE: GRAFTS AND FLAPS
Various
surgical techniques, including skin grafts and flaps, are used to cover skin
wounds.
Skin Grafts
Skin grafting is a technique in which a section of skin is detached from its own blood supply and transferred as free tissue to a dis-tant (recipient) site. Skin grafting can be used to repair almost any type of wound and is the most common form of reconstructive surgery.
Skin
grafts are commonly used to repair defects that result from excision of skin
tumors, to cover areas denuded of skin (e.g., burns), and to cover wounds in
which insufficient skin is available to permit wound closure. They are also
used when primary closure of the wound increases the risk for complica-tions or
when primary wound closure would interfere with function.
Skin grafts may be classified as autografts,
allografts, or xenografts. An autograft is tissue obtained from the patient’s
own skin. An allograft is tissue obtained from a donor of the same species.
These grafts are also called allogeneic or homograft. A xenograft or
heterograft is tissue from another species.
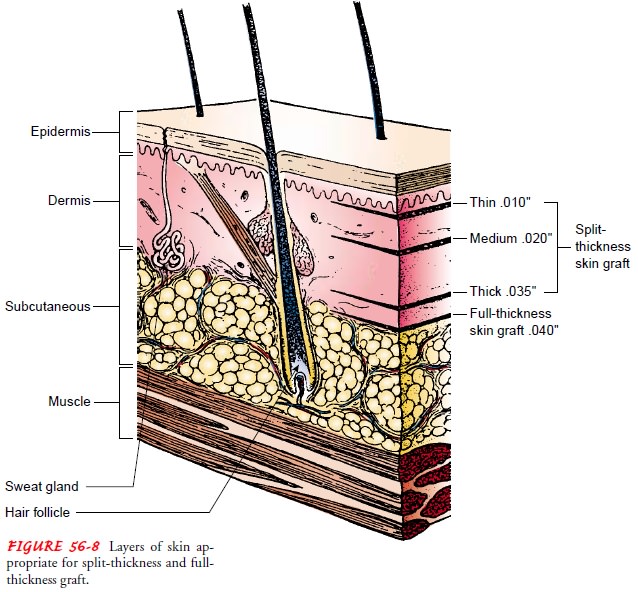
Grafts
are also referred to by their thickness. A skin graft may be a split-thickness
(ie, thin, intermediate, or thick) or full-thickness graft, depending on the
amount of dermis included in the specimen. A split-thickness graft can be cut
at various thick-nesses and is commonly used to cover large wounds or defects
for which a full-thickness graft or flap is impractical (Fig. 56-8). A
full-thickness graft consists of epidermis and the entire dermis without the
underlying fat. It is used to cover wounds that are too large to be closed
directly.
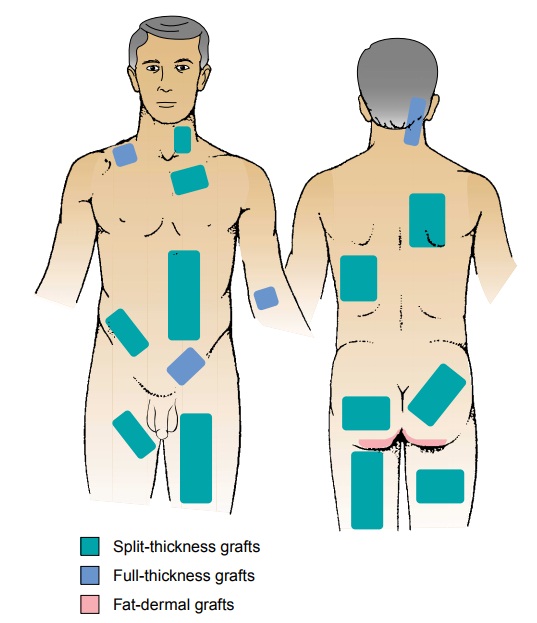
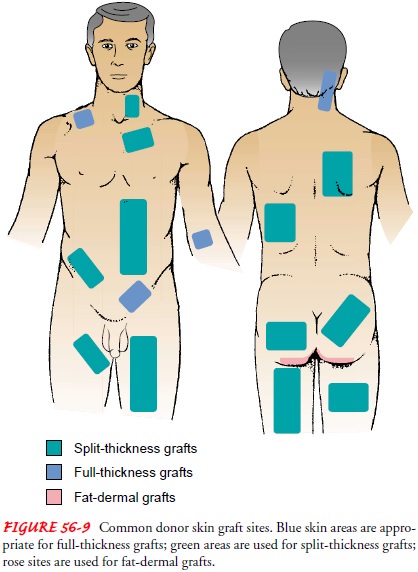
DONOR SITE
The
donor site is selected with several criteria in mind:
·
Achieving the closest possible
color match
·
Matching the texture and
hair-bearing qualities
·
Obtaining the thickest
possible skin graft without jeopar-dizing the healing of the donor site (Fig.
56-9)
·
Considering the cosmetic
effects of the donor site after heal-ing, so that it is in an inconspicuous
location
DONOR SITE CARE
Detailed attention to the donor site is just as
important as the care of the recipient area. The donor site heals by
re-epithelization of the raw, exposed dermis. Usually, a single layer of
nonadherent, fine-mesh gauze is placed directly over the donor site. Absorbent
gauze dressings are then placed on top to absorb blood or serum from the wound.
A membrane dressing (eg, Op-Site) may be used and pro-vides certain advantages.
It is transparent and allows the wound to be observed without disturbing the
dressing, and it permits the pa-tient to shower without fear of saturating the
dressing with water.
After
healing, the patient is instructed to keep the donor site soft and pliable with
cream (eg, lanolin, olive oil). Extremes in temperature, external trauma, and
sunlight are to be avoided for donor sites and grafted areas because these
areas are sensitive, especially to thermal injuries.
GRAFT APPLICATION
A
graft is obtained by a variety of instruments: razor blades, skin-grafting
knives, electric- or air-powered dermatomes, or drum der-matomes. The skin
graft is taken from the donor or host site and applied to the desired site,
called the recipient site or graft bed.
For
a graft to survive and be effective, certain conditions must be met:
·
The recipient site must have
an adequate blood supply so that normal physiologic function can resume.
·
The graft must be in close
contact with its bed to avoid ac-cumulation of blood or fluid.
·
The graft must be fixed firmly
(immobilized) so that it re-mains in place on the recipient site.
·
The area must be free of
infection.
The graft, when applied to the recipient site, may
be sutured in place. It may be slit and spread apart to cover a greater area.
The process of revascularization (ie, establishing the blood sup-ply) and
reattachment of a skin graft to a recipient bed is referred to as a “take.”
After a skin graft is put in place, it may be left ex-posed (in areas that are
impossible to immobilize) or covered with a light dressing or a pressure
dressing, depending on the area.
Nursing Interventions
The
nurse instructs the patient to keep the affected part immo-bilized as much as
possible. For a facial graft, strenuous activity must be avoided. A graft on
the hand or arm may be immobilized with a splint. When a graft is placed on a
lower extremity, the part is kept elevated because the new capillary
connections are fragile and excess venous pressure may cause rupture. When
ambulation is permitted, the patient wears an elastic stocking to
counter-balance venous pressure.
The
nurse instructs the patient, family member, or other care-giver to inspect the
dressing daily. Unusual drainage or an in-flammatory reaction around the wound
margin suggests infection and should be reported to the physician. Any fluid,
purulent drainage, blood, or serum that has collected is gently evacuated by
the surgeon, because accumulation of this material would cause the graft to
separate from its bed.
When
the graft appears pink, it is vascularized. After 2 to 3 weeks, mineral oil or
a lanolin cream is massaged into the wound to moisten the graft. Because there
may be loss of feeling or sen-sation in the grafted area for a prolonged
period, the application of heating pads and exposure to sun are avoided to
prevent burns and further skin trauma.
Flaps
Another
form of wound coverage is provided by flaps. A flap is a segment of tissue that
remains attached at one end (ie, a base or pedicle) while the other end is
moved to a recipient area. Its sur-vival depends on functioning arterial and
venous blood supplies and lymphatic drainage in its pedicle or base. A flap
differs from a graft in that a portion of the tissue is attached to its
original site and retains its blood supply. An exception is the free flap,
which is described later.
Flaps
may consist of skin, mucosa, muscle, adipose tissue, omentum, and bone. They
are used for wound coverage and pro-vide bulk, especially when bone, tendon,
blood vessels, or nerve tissue is exposed. Flaps are used to repair defects
caused by con-genital deformity, trauma, or tumor ablation (ie, removal,
usu-ally by excision) in an adjacent part of the body.
Flaps
offer an aesthetic solution because a flap retains the color and texture of the
donor area, is more likely to survive than a graft, and can be used to cover
nerves, tendons, and blood vessels. However, several surgical procedures are
usually required to ad-vance a flap. The major complication is necrosis of the
pedicle or base as a result of failure of the blood supply.
Free Flaps
A striking advance in reconstructive surgery is the
use of free flaps or free-tissue transfer achieved by microvascular techniques.
A free flap is completely severed from the body and transferred to another
site. A free flap receives early vascular supply from micro-vascular
anastomosis (ie, attachment) with vessels at the recipient site. The procedure
usually is completed in one step, eliminating the need for a series of surgical
procedures to move the flap. Micro-vascular surgery allows surgeons to use a
variety of donor sites for tissue reconstruction.
Related Topics