Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Nursing Process: Care of the Patient With Psoriasis
NURSING PROCESS:CARE OF THE PATIENT WITH PSORIASIS
Assessment
The
nursing assessment focuses on how the patient is coping with the psoriatic skin
condition, appearance of the normal skin, and appearance of the skin lesions,
as described previously. The notable manifestations are red, scaling papules
that coalesce to form oval, well-defined plaques. Silver-white scales may also
be present. Adjacent skin areas show red, smooth plaques with a macerated
surface. It is important to examine the areas especially prone to psoriasis:
elbows, knees, scalp, gluteal cleft, fingers, and toenails (for small pits).
Psoriasis
may cause despair and frustration for the patient; ob-servers may stare,
comment, ask embarrassing questions, or even avoid the person. The disease can eventually
exhaust the patient’s resources, interfere with his or her job, and make life
miserable in general. Teenagers are especially vulnerable to the psychological
effects of this disorder. The family, too, is affected, because time-consuming
treatments, messy salves, and constant shedding of scales may disrupt home life
and cause resentment. The patient’s frustrations may be expressed through
hostility directed at health care personnel and others.
The
nurse assesses the impact of the disease on the patient and the coping
strategies used for conducting normal activities and interactions with family
and friends. Many patients need reas-surance that the condition is not
infectious, not a reflection of poor personal hygiene, and not skin cancer.
Diagnosis
NURSING DIAGNOSES
Based
on the nursing assessment data, the patient’s major nurs-ing diagnoses may
include the following:
·
Deficient knowledge about the
disease process and treat-ment
·
Impaired skin integrity
related to lesions and inflammatory response
·
Disturbed body image related
to embarrassment over ap-pearance and self-perception of uncleanliness
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications include the following:
·
Infection
·
Psoriatic arthritis
Planning and Goals
Major
goals for the patient may include increased understanding of psoriasis and the
treatment regimen, achievement of smoother skin with control of lesions,
development of self-acceptance, and absence of complications.
Nursing Interventions
PROMOTING UNDERSTANDING
The nurse explains with sensitivity that, although
there is no cure for psoriasis and lifetime management is necessary, the
condition can usually be controlled. The pathophysiology of psoriasis is
re-viewed, as are the factors that provoke it—irritation or injury to the skin
(eg, cut, abrasion, sunburn), current illness (eg, pharyn-geal streptococcal
infection), and emotional stress. It is empha-sized that repeated trauma to the
skin and an unfavorable environment (eg, cold) or a specific medication (eg,
lithium, beta-blockers, indomethacin) may exacerbate psoriasis. The patient is
cautioned about taking any nonprescription medications because some may
aggravate mild psoriasis.
Reviewing and explaining the treatment regimen are
essential to ensure compliance. For example, if the patient has a mild
con-dition confined to localized areas, such as the elbows or knees,
ap-plication of an emollient to maintain softness and minimize scaling may be
all that is required. However, if the patient uses anthralin, the dosage
schedule, possible side effects, and problems to report to the nurse or
physician should be explained.
Most
patients need a comprehensive plan of care that ranges from using topical
medications and shampoos to more complex and lengthy treatment with systemic
medications and photo-chemotherapy, such as PUVA therapy. Patient education
materials that include a description of the therapy and specific guidelines are
helpful but cannot replace face-to-face discussions of the treat-ment plan.
INCREASING SKIN INTEGRITY
To avoid injuring the skin, the patient is advised
not to pick at or scratch the affected areas. Measures to prevent dry skin are
en-couraged because dry skin worsens psoriasis. Too-frequent wash-ing produces
more soreness and scaling. Water should be warm, not hot, and the skin should
be dried by patting with a towel rather than by rubbing. Emollients have a
moisturizing effect, providing an occlusive film on the skin surface so that
normal water loss through the skin is halted and allowing the
trapped water to hydrate the stratum corneum. A bath oil or emollient cleansing
agent can comfort sore and scaling skin. Softening the skin can prevent
fissures (see Plan of Nursing Care 56-1).
IMPROVING SELF-CONCEPT AND BODY IMAGE
A therapeutic relationship between health care
professionals and the patient with psoriasis is one that includes education and
sup-port. After the treatment regimen is established, the patient should begin
to feel more confident and empowered in carrying it out and in using coping
strategies that help deal with the altered self-concept and body image brought
about by the disease. Introducing the patient to successful coping strategies
used by others with pso-riasis and making suggestions for reducing or coping
with stress-ful situations at home, school, and work can facilitate a more
positive outlook and acceptance of the chronicity of the disease.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Psoriatic Arthritis
The diagnosis of psoriasis, especially when it is
accompanied by the complication of arthritis, is usually difficult to make.
Psoriatic arthritis involving the sacroiliac and distal joints of the fingers
may be overlooked, especially if the patient has the typical psoriatic
le-sions. However, patients who complain of mild joint discomfort and some
pitting of the fingernails may not be diagnosed with pso-riasis until the more
obvious cutaneous lesions appear.
The
complaint of joint discomfort in the patient with psoria-sis should be noted
and evaluated. The symptoms of psoriatic arthritis can mimic the symptoms of
Reiter’s disease and anky-losing spondylitis, and a definitive diagnosis must
be made. Treat-ment of the condition usually involves joint rest, application
of heat, and salicylates.
The patient requires education about the care and
treatment of the involved joints and the need for compliance with therapy. The
incidence of psoriatic arthropathy is unknown because the symp-toms are so
variable. It is believed, however, that when the psoriasis is extensive and a
family history of inflammatory arthritis is elicited, the chance that the
patient will develop psoriatic arthritis increases substantially. It is
recommended that a rheumatologist be consulted to assist in the diagnosis and treatment
of the arthropathy.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Printed patient education materials may be provided
to reinforce face-to-face discussions about treatment guidelines and other
considerations. For example, the patient and the family caregiver may need to
know that the topical agent anthralin leaves a brownish purple stain on the
skin but that the discoloration subsides after an-thralin treatment stops. The
patient should also be instructed to cover lesions treated with anthralin with
gauze, stockinette, or other soft coverings to avoid staining clothing,
furniture, and bed linens.
Patients
using topical corticosteroid preparations repeatedly on the face and around the
eyes should be aware that cataract de-velopment is possible. Strict guidelines
for applying these med-ications should be emphasized because overuse can result
in skin atrophy, striae, and medication resistance.
Photochemotherapy (PUVA), which is reserved for
moderate to severe psoriasis, produces photosensitization, which means that the
skin is sensitive to the sun until methoxsalen has been ex-creted from the body
in about 6 to 8 hours. Patients undergoing PUVA treatments should avoid
exposure to the sun. If exposure is unavoidable, the skin must be protected
with sunscreen and clothing. Gray- or green-tinted, wraparound sunglasses
should be worn to protect the eyes during and after treatment, and
oph-thalmologic examinations should be performed on a regular basis. Nausea,
which may be a problem in some patients, is lessened when methoxsalen is taken
with food. Lubricants and bath oils may be used to help remove scales and
prevent excessive dryness. No other creams or oils are to be used except on
areas that have been shielded from ultraviolet light. Contraceptives should be
used by sexually active women of reproductive age, because the teratogenic
effect of PUVA has not been determined. The patient is kept under constant and
careful supervision and is encouraged to recognize unusual changes in the skin.
If
indicated, referral may be made to a mental health profes-sional who can help
to ease emotional strain and give support. Be-longing to a support group may
also help patients acknowledge that they are not alone in experiencing life
adjustments in re-sponse to a visible, chronic disease. The National Psoriasis
Foun-dation publishes periodic bulletins and reports about new and relevant
developments in this condition.
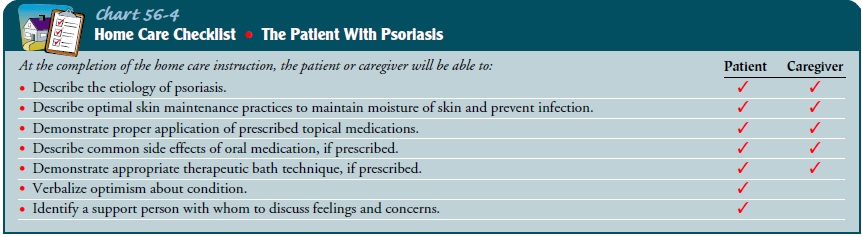
Chart
56-4 is a Home Care Checklist for the patient with psoriasis.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
1) Demonstrates
knowledge and understanding of disease process and its treatment
a) Describes
psoriasis and the prescribed therapy
b) Verbalizes that trauma, infection, and emotional stress may be trigger factors
c) Maintains
control with appropriate therapy
d) Demonstrates
proper application of topical therapy
2) Achieves
smoother skin and control of lesions
a) Exhibits
no new lesions
b) Keeps
skin lubricated and soft
3) Develops
self-acceptance
a) Identifies
someone with whom to discuss feelings and concerns
b) Expresses
optimism about outcomes of treatment
4) Absense
of complications
a) Has
no joint discomfort
b) Reports
control of cutaneous lesions with no extension of disease
Related Topics