Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Wound Care for Skin Conditions
Wound Care for Skin Conditions
There
are three major classifications of dressings for skin condi-tions: wet,
moisture-retentive, and occlusive. During the 1980s and 1990s, new product
development quadrupled the available choices for wound care, especially within
the moisture-retentive dressing classification. Products classified as
moisture-retentive dressings include hydrogels, foams, and alginates.
Biologicals and biosynthetics containing collagen and growth factor are being
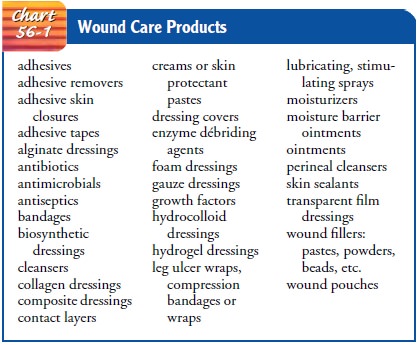
researched and will soon be available. Chart 56-1 lists generic wound care
products. Consultation with a wound care specialist can be very helpful in
choosing the product most appropriate for the patient.
Dressings and Rules of Wound Care
Even
with the increased availability of dressings, an appropriate selection can be
made if certain principles are maintained, re-ferred to as the five rules of
wound care (Krastner, et al, 2002).
Rule 1: Categorization.
The nurse should learn about dressingsby generic category and compare new
products with those that already make up the category. As hundreds of choices
become available, the nurse should become familiar with the generic cat-egories
and develop a systematic approach to product selection. The nurse should become
familiar with indications, contra-indications, and side effects. The best
dressing may be created by combining products in different categories to
achieve several goals at the same time. These categories are discussed in sub-sequent
sections.
Rule 2: Selection.
The nurse should select the safest and mosteffective, user-friendly, and cost-effective dressing possible. In many cases, nurses carry out the physician’s prescriptions for dressings, but they should be prepared to give the physician feed-back about the dressing’s effect on the wound, ease of use for the patient, and other considerations when applicable.
Rule 3: Change.
The nurse changes dressings based on patient,
wound, and dressing assessments, not on standardized routines. Traditional
nursing care plans recommended changing dressings on a routine schedule, often
three or four times each day.
Rule 4: Evolution.
As the wound progresses through the phasesof wound healing, the dressing
protocol is altered to optimize wound healing. It is rare, especially in cases
of chronic wounds, that the same dressing material is appropriate throughout
the healing process. The rule assumes that the nurse and the patient or family
have access to a wide variety of products and knowledge about their use. The
nurse teaches the patient or family caregiver about wound care and ensures that
the family has access to ap-propriate dressing choices.
Rule 5: Practice.
Practice with dressing material is required forthe nurse to learn the
performance parameters of the particular dressing. Refining the skills of
applying appropriate dressings cor-rectly and learning about new dressing
products are essential nursing responsibilities. Dressing changes should not be
dele-gated to assistive personnel; these techniques require the knowl-edge base
and assessment skills of professional nurses.
Wet Dressings
Wet dressings (ie, wet compresses applied to the
skin) were tra-ditionally used for acute, weeping, inflammatory lesions. They
have become almost obsolete in light of the many newer products available for
wound care. Wet dressings are sterile or nonsterile (clean), depending on the
skin disorder. They are used to reduce inflammation by producing constriction
of the blood vessels (thereby decreasing vasodilation and local blood flow in
inflam-mation); to clean the skin of exudates, crusts, and scales; to main-tain
drainage of infected areas; and to promote healing by facilitating the free
movement of epidermal cells across the in-volved skin so that new granulation
tissue forms. Wet dressings can be used for vesicular, bullous, pustular, and
ulcerative disor-ders, as well as for inflammatory conditions.
Before applying these dressings, the nurse performs
hand hy-giene and puts on sterile or clean gloves. The open dressing requires
frequent changes because evaporation is rapid. The closed dress-ing is changed
less frequently, but there is always a danger that the closed dressing may
cause not only softening and but actual maceration of the underlying skin.
Wet-to-dry dressings are used to remove exudate from erosions or ulcers. The
dressing remains in place until it dries. It is then removed without soaking so
that crusts, exudate, or pus from the skin lesion adhere to the dressing and are
removed with it.
Moisture-Retentive Dressings
Newer, commercially produced moisture-retentive
dressings can perform the same functions as wet compresses but are more
effi-cient at removing exudate because of their higher moisture-vapor
transmission rate; some have reservoirs that can hold excessive ex-udate. There
is also evidence that moist wound healing results in wound resurfacing 40%
faster than with air exposure. A number of moisture-retentive dressings are
already impregnated with saline solution, petrolatum, zinc-saline solution,
hydrogel, or anti-microbial agents, thereby eliminating the need to coat the
skin to avoid maceration. The main advantages of moisture-retentive dressings
over wet compresses are reduced pain, fewer infections, less scar tissue,
gentle autolytic débridement, and decreased fre-quency of dressing changes.
Depending on the product used and the type of dermatologic problem encountered,
most moisture-retentive dressings may remain in place from 12 to 24 hours; some
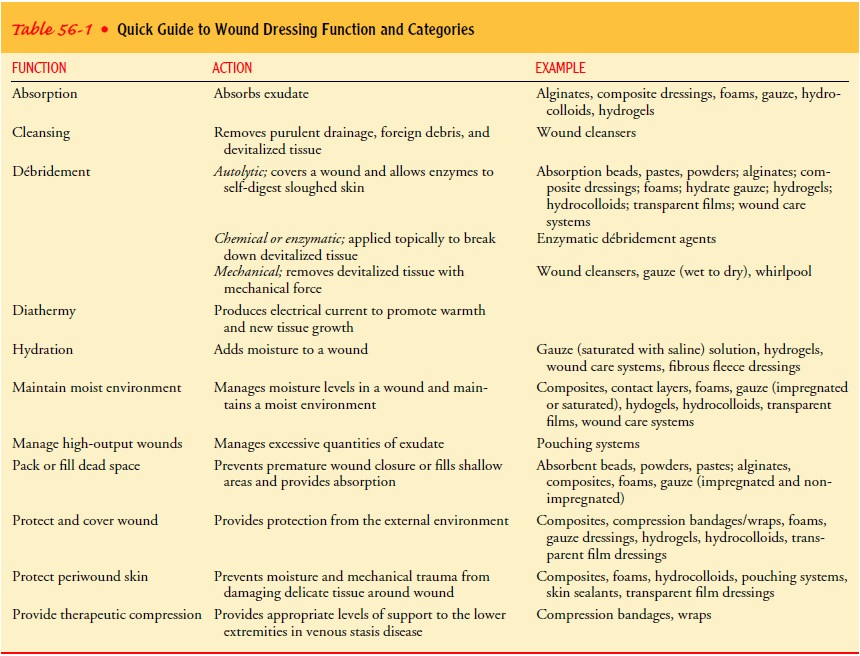
can remain in place as long as a week. Table 56-1 is a guide to wound dressing
functions and categories.
Hydrogels are polymers with a 90% to 95% water
content. They are available in impregnated sheets or as gel in a tube. Their
high moisture content makes them ideal for autolytic débride-ment of wounds.
They are semitransparent, allowing for wound inspection without dressing
removal. They are comfortable and soothing for the painful wound. They have no
inherent adhesive and require a secondary dressing to keep them in place.
Hydro-gels are appropriate for superficial wounds with high serous out-put,
such as abrasions, skin graft sites, and draining venous ulcers.
Hydrocolloids are composed of a water-impermeable,
poly-urethane outer covering separated from the wound by a hydro-colloid
material. They are adherent and nonpermeable to water vapor and oxygen. As it
evaporates over the wound, water is ab-sorbed into the dressing, which softens
and discolors with the increased water content. The dressing can be removed without
damage to the wound. As the dressing absorbs water, it produces a
foul-smelling, yellowish covering over the wound. This is a normal chemical
interaction between the dressing and wound exudate and should not be confused
with purulent drainage from the wound. Unfortunately, most of the hydrocolloid
dressings are opaque, lim-iting inspection of the wound without removal of the
dressing.
Available in sheets and in gels, hydrocolloids are a good choice for exudative wounds and for acute wounds. Easy to use and comfortable, hydrocolloid dressings promote débridement and formation of granulation tissue. They do not have to be removed for bathing. Most can be left in place for up to 7 days.
Foam
dressings consist of microporous polyurethane with an absorptive hydrophilic (ie, water-absorbing)
surface that covers the wound and a hydrophobic
(ie, water-resistant) backing to block leakage of exudate. They are nonadherent
and require a secondary dressing to keep them in place. Moisture is absorbed
into the foam layer, decreasing maceration of surrounding tis-sue. A moist
environment is maintained, and removal of the dressing does not damage the
wound. The foams are opaque and must be removed for wound inspection. Foams are
a good choice for exudative wounds. They are especially helpful over bony
prominences because they provide contoured cushioning.
Calcium
alginates are derived from seaweed and consist of tremendously absorbent
calcium alginate fibers. They are hemo-static and bioabsorbable and can be used
as sheets, mats, or ropes of absorbent material. As the exudate is absorbed,
the fibers turn into a viscous hydrogel. They are quite useful in areas where
the tissue is more irritated or macerated. The alginate dressing forms a moist
pocket over the wound while the sur-rounding skin stays dry. They also react
with wound fluid to form a foul-smelling coating. Alginates work well when
packed into a deep cavity, wound, or sinus tract with heavy drainage (Krastner
et al, 2002). They are nonadherent and require a secondary dressing.
Occlusive Dressings
Occlusive dressings may be commercially produced or
made in-expensively from sterile or nonsterile gauze squares or wrap. Occlusive
dressings cover topical medication that is applied to a dermatosis (ie, abnormal skin lesion). The area is kept airtightby
using plastic film (eg, plastic wrap). Plastic film is thin and readily adapts
to all sizes, body shapes, and skin surfaces. Plastic surgical tape containing
a corticosteroid in the adhesive layer can be cut to size and applied to
individual lesions. Generally, plastic wrap should be used no more than 12
hours each day.
AUTOLYTIC DÉBRIDEMENT
Autolytic débridement
is a process that uses the body’s own digestive enzymes to break down necrotic
tissue. The wound is kept moist with occlusive dressings. Eschar and necrotic
debris are softened, liquefied, and separated from the bed of the wound.
Several commercially available products contain the
same en-zymes that the body produces naturally. These are called enzy-matic
débriding agents; examples include Accu Zyme, collagenase (Santyl), Granulex,
and Zymase. Application of these products speeds the rate at which necrotic
tissue is removed. This method is still slower and no more effective than
surgical débridement. When enzymatic débridment is being used under an
occlusivedressing, a foul odor is produced by the breakdown of
cellular de-bris. This odor does not indicate that the wound is infected. The
nurse should expect this reaction, and help the patient under-stand the reason
for the odor.
Advances in Wound Treatment
Increasing understanding of how skin heals has led
to several ad-vances in therapy. Growth factors are cytokines or proteins that
have potent mitogenic activity (Valencia et al., 2001). Low levels of cytokines
circulate in the blood continuously, but activated platelets release increased
amounts of preformed growth factors into a wound. This increase in cytokines in
the wound stimulates cellular growth and granulation of skin. Regranex gel
contains be-caplermin, a platelet-derived growth factor, which is applied to
the wound to stimulate healing. Apligraf is a skin construct (ie,
bio-engineered skin substitute) imbedded in a dressing that also con-tains
cytokines and fibroblasts. When applied to wounds, these agents stimulate
platelet activity and potentially decrease wound healing time (Paquette &
Falanga, 2002).
Some oral medications are being investigated for
their bene-fits in healing chronic venous ulcers of the lower legs. Pentoxi-fylline
(Trental) increases peripheral blood flow by decreasing the viscosity of blood.
It has some fibrinolytic action and decreases leukocyte adhesion to the wall of
the blood vessels. Enteric-coated aspirin has also been shown to be of value,
although its exact mechanism is still not clear (Valencia et al., 2001).
Medical Management
THERAPEUTIC BATHS (BALNEOTHERAPY)AND MEDICATIONS
Baths
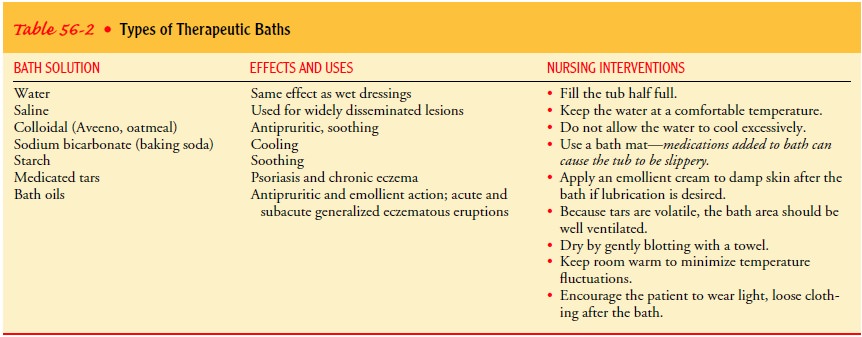
or soaks, known as balneotherapy,
are useful when large areas of skin are affected. The baths remove crusts,
scales, and old medications and relieve the inflammation and itching that
ac-company acute dermatoses. The water temperature should be comfortable, and
the bath should not exceed 20 to 30 minutes because of the tendency of baths
and soaks to produce skin mac-eration. Table 56-2 lists the different types of
therapeutic baths and their uses.
PHARMACOLOGIC THERAPY
Because skin is easily accessible and therefore
easy to treat, topi-cal medications are often used. High concentrations of some
medications can be applied directly to the affected site with little systemic
absorption and therefore with few systemic side effects. However, some
medications are readily absorbed through the skin and can produce systemic
effects. Because topical prepara-tions may induce allergic contact dermatitis (ie, inflammation of the
skin) in sensitive patients, any untoward response should be reported
immediately and the medication discontinued.
Medicated lotions, creams, ointments, and powders
are fre-quently used to treat skin lesions. In general, moisture-retentive
dressings, with or without medication, are used in the acute stage; lotions and
creams are reserved for the subacute stage; and oint-ments are used when
inflammation has become chronic and the skin is dry with scaling or lichenification (ie, leathery
thickening).
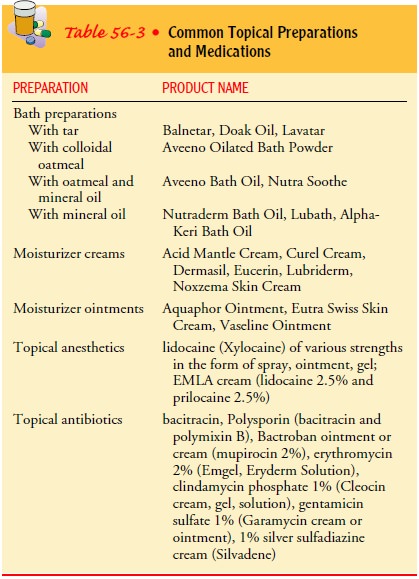
With
all types of topical medication, the patient is taught to apply the medication
gently but thoroughly and, when neces-sary, to cover the medication with a
dressing to protect clothing. Table 56-3 lists some commonly used topical
preparations.
Lotions.
Lotions are of two types: suspensions and
liniments. Sus-pensions consist of a powder in water, requiring shaking before
application, and clear solutions, containing completely dissolved active
ingredients. Lotions are usually applied directly to the skin, but a dressing
soaked in the lotion can be placed on the affected area. A suspension such as
calamine lotion provides a rapid cool-ing and drying effect as it evaporates,
leaving a thin, medicinal layer of powder on the affected skin. Lotions are
frequently used to replenish lost skin oils or to relieve pruritus. Lotions
must be applied every 3 or 4 hours for sustained therapeutic effect. If left in
place for a longer period, they may crust and cake on the skin. Liniments are
lotions with oil added to prevent crusting. Because lotions are easy to use,
therapeutic compliance is generally high.
Powders.
Powders usually have a talc, zinc oxide, bentonite, orcornstarch base and are dusted on the skin with a shaker or with cotton sponges. Although their therapeutic action is brief, pow-ders act as hygroscopic agents that absorb and retain moisture from the air and reduce friction between skin surfaces and cloth-ing or bedding.
Creams.
Creams may be suspensions of oil in water or
emulsions of water in oil, with additional ingredients to prevent bacterial and
fungal growth. Both may cause an allergic reaction such as contact dermatitis.
Oil-in-water creams are easily applied and usually are the most cosmetically
acceptable to the patient. Although they can be used on the face, they tend to
have a drying effect. Water-in-oil emulsions are greasier and are preferred for
drying and flaking dermatoses. Creams usually are rubbed into the skin by hand.
They are used for their moisturizing and emollient effects.
Gels.
Gels are semisolid emulsions that become liquid when
ap-plied to the skin or scalp. They are cosmetically acceptable to the patient
because they are not visible after application, and they are greaseless and
nonstaining. The newer water-based gels appear to penetrate the skin more
effectively and cause less stinging on ap-plication. They are especially useful
for acute dermatitis in which there is weeping exudate (eg, poison ivy).
Pastes.
Pastes are mixtures of powders and ointments and areused in inflammatory
blistering conditions. They adhere to the skin and may be difficult to remove
without using an oil (eg, olive oil, mineral oil). Pastes are applied with a
wooden tongue depressor or gloved hand.
Ointments.
Ointments retard water loss and lubricate and pro-tect the skin. They are
the preferred vehicle for delivering med-ication to chronic or localized dry
skin conditions, such as eczema or psoriasis. Ointments are applied with a
wooden tongue de-pressor or by hand (gloved).
Sprays and Aerosols.
Spray and aerosol preparations may beused on any widespread dermatologic
condition. They evaporate on contact and are used infrequently.
Corticosteroids.
Corticosteroids are widely used in treating
der-matologic conditions to provide anti-inflammatory, antipruritic, and
vasoconstrictive effects. The patient is taught to apply this medication
according to strict guidelines, using it sparingly but rubbing it into the
prescribed area thoroughly. Absorption of top-ical corticosteroid is enhanced
when the skin is hydrated or the affected area is covered by an occlusive or
moisture-retentive dressing. Inappropriate use of topical corticosteroids can
result in local and systemic side effects, especially when the medication is
absorbed through inflamed and excoriated skin, under occlusive dressings, or
when used for long periods on sensitive areas. Local side effects may include
skin atrophy and thinning, striae (ie, band-like streaks), and telangiectasia.
Thinning of the skin results from the ability of corticosteroids to inhibit
skin collagen synthesis (Odom et al., 2000). The thinning process can be
reversed by discontinuing the medication, but striae and telangiectasia are
per-manent. Systemic side effects may include hyperglycemia and symptoms of
Cushing’s syndrome. Caution is required when ap-plying corticosteroids around
the eyes because long-term use may cause glaucoma or cataracts, and the
anti-inflammatory effect of corticosteroids may mask existing viral or fungal
infections.
Concentrated
(fluorinated) corticosteroids are never applied on the face or intertriginous
areas (ie, axilla and groin), because these areas have a thinner stratum
corneum and absorb the med-ication much more quickly than areas such as the
forearm or legs. Persistent use of concentrated topical corticosteroids in any
loca-tion may produce acnelike dermatitis, known as steroid-induced acne, and
hypertrichosis (ie, excessive hair growth). Because some topical corticosteroid
preparations are available without pre-scription, patients should be cautioned
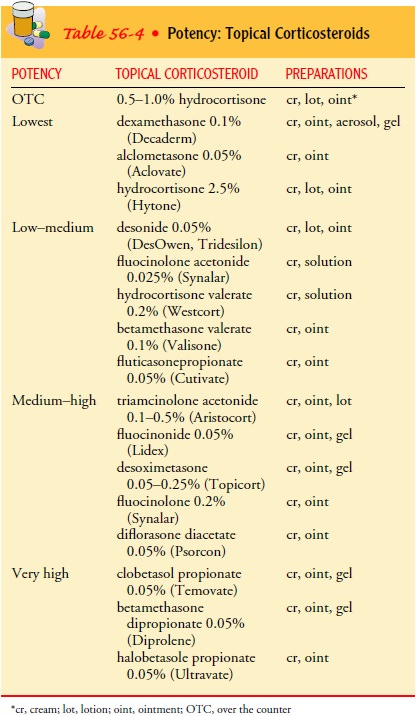
about prolonged and in-appropriate use. Table 56-4 lists topical corticosteroid
preparations according to potency.
Intralesional Therapy.
Intralesional therapy consists of injectinga sterile suspension of
medication (usually a corticosteroid) into or just below a lesion. Although
this treatment may have an anti-inflammatory effect, local atrophy may result
if the medication is injected into subcutaneous fat. Skin lesions treated with
in-tralesional therapy include psoriasis, keloids, and cystic acne.
Occasionally, immunotherapeutic and antifungal agents are ad-ministered as
intralesional therapy.
Systemic Medications.
Systemic medications are also prescribed for skin
conditions. These include corticosteroids for short-term therapy for contact
dermatitis or for long-term treatment of a chronic dermatosis, such as
pemphigus vulgaris. Other frequently used systemic medications include
antibiotics, antifungals, anti-histamines, sedatives, tranquilizers,
analgesics, and cytotoxic agents.
Nursing Management
Management begins with a health history, direct observation, and a complete physical examination. Because of its visibility, a skin condition is usually difficult to ignore or conceal from others and may therefore cause the patient some emotional distress. The major goals for the patient may include maintenance of skin integrity, relief of discomfort, promotion of restful sleep, self-acceptance, knowledge about skin care, and avoidance of complications.
Nursing
management for patients who must perform self-care for skin problems, such as
applying medications and dressings, focuses mainly on teaching the patient how
to wash the affected area and pat it dry, apply medication to the lesion while
the skin is moist, cover the area with plastic (eg, Telfa pads, plastic wrap,
vinyl gloves, plastic bag) if recommended, and cover it with an elastic
bandage, dressing, or paper tape to seal the edges. Dressings that contain or
cover a topical corticosteroid should be removed for 12 of every 24 hours to
prevent skin thinning (ie, atrophy), striae, and telangiectasia (ie, small, red
lesions caused by dilation of blood vessels).
Other forms of dressings, such as those used to
cover topical medications, include soft cotton cloth and stretchable cotton
dress-ings (eg, Surgitube, TubeGauz) that can be used for fingers, toes, hands,
and feet. The hands can be covered with disposable poly-ethylene or vinyl gloves
sealed at the wrists; the feet can be wrapped in plastic bags covered by cotton
socks. Gloves and socks that are already impregnated with emollients, making
application to the hands and feet more convenient, are also available. When
large areas of the body must be covered, cotton cloth topped by an ex-pandable
stockinette can be used. Disposable diapers or cloths folded in diaper fashion
are useful for dressing the groin and the perineal
areas. Axillary dressings can be made of cotton cloth, or a commercially
prepared dressing may be used and taped in place or held by dress shields. A
turban or plastic shower cap is useful for holding dressings on the scalp. A
face mask, made from gauze with holes cut out for the eyes, nose, and mouth,
may be held in place with gauze ties looped through holes cut in the four
corners of the mask. See the Plan of Nursing Care 56-1 for more information.
Related Topics