Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Pruritus
Pruritus
GENERAL ITCHING
Pruritus
(ie, itching) is one of the most common symptoms of patients with dermatologic
disorders. Itch receptors are unmyeli-nated, penicillate (ie, brushlike) nerve
endings that are found ex-clusively in the skin, mucous membranes, and cornea.
Although pruritus is usually caused by primary skin disease with resultant rash
or lesions, it may occur without a rash or lesion. This is re-ferred to as
essential pruritus, which generally has a rapid onset, may be severe, and
interferes with normal daily activities.
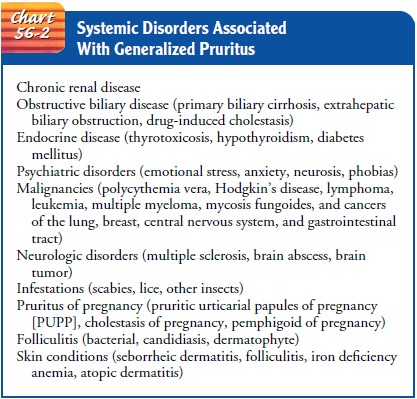
Pruritus
may be the first indication of a systemic internal dis-ease such as diabetes mellitus,
blood disorders, or cancer. It may also accompany renal, hepatic, and thyroid
diseases (Chart 56-2). Some common oral medications such as aspirin,
antibiotics, hor-mones (ie, estrogens, testosterone, or oral contraceptives),
and opioids (ie, morphine or cocaine) may cause pruritus directly or by
increasing sensitivity to ultraviolet light. Certain soaps and chemicals,
radiation therapy, prickly heat (ie, miliaria), and con-tact with woolen
garments are also associated with pruritus. Pru-ritus may also be caused by
psychological factors, such as excessive stress in family or work situations.
Pathophysiology
Scratching
the itchy area causes the inflamed cells and nerve end-ings to release
histamine, which produces more pruritus, gener-ating a vicious itch–scratch
cycle. If the patient responds to an itch by scratching, the integrity of the
skin may be altered, and excoriation, redness, raised areas (ie, wheals),
infection, or changes in pigmentation may result. Pruritus usually is more
severe at night and is less frequently reported during waking hours, prob-ably
because the person is distracted by daily activities. At night, when there are
few distractions, the slightest pruritus cannot be easily ignored. Severe
itching is debilitating.
Gerontologic Considerations
Pruritus occurs frequently in elderly people as a
result of dry skin. Elderly people are also more likely to have a systemic
illness that triggers pruritus, are at higher risk for occult malignancy, and
are more likely to be on multiple medications than is the younger population.
All of these factors increase the incidence of pruritus.
Medical Management
A thorough history and physical examination usually provide clues to the underlying cause of the pruritus, such as hay fever, allergy, recent administration of a new medication, or a change of cos-metics or soaps. After the cause has been identified, treatment of the condition should relieve the pruritus. Signs of infection and environmental clues, such as warm, dry air or irritating bed linens, should be identified. In general, washing with soap and hot water is avoided.
Bath oils (eg, Lubath, Alpha-Keri) containing a sur-factant that makes
the oil mix with bath water may be sufficient for cleaning. However, an elderly
patient or a patient with un-steady balance should avoid adding oil because it
increases the danger of slipping in the bathtub. A warm bath with a mild soap
followed by application of a bland emollient to moist skin can control xerosis
(ie, dry skin). Applying a cold compress, ice cube, or cool agents that contain
menthol and camphor (which constrict blood vessels) may also help relieve
pruritus.
PHARMACOLOGIC THERAPY
Topical corticosteroids may be beneficial as anti-inflammatory agents to decrease itching. Oral antihistamines are even more ef-fective because they can overcome the effects of histamine release from damaged mast cells. An antihistamine, such as diphenhy-dramine (Benadryl) or hydroxyzine (Atarax), prescribed in a seda-tive dose at bedtime is effective in producing a restful and comfortable sleep.
Nonsedating antihistamine medications such as fexofenadine (Allegra) should be used to relieve
daytime pru-ritus. Tricyclic antidepressants, such as doxepin (Sinequan), may
be prescribed for pruritus of neuropsychogenic origin. If pruritus continues,
further investigation of a systemic problem is advised.
Nursing Management
The
nurse reinforces the reasons for the prescribed therapeutic regimen and
counsels the patient on specific points of care. If baths have been prescribed,
the patient is reminded to use tepid (not hot) water and to shake off the
excess water and blot between intertriginous areas (ie, body folds) with a
towel. Rubbing vigor-ously with the towel is avoided because this
overstimulates the skin and causes more itching. It also removes water from the
stra-tum corneum. Immediately after bathing, the skin should be lu-bricated
with an emollient to trap moisture.
The patient is instructed to avoid situations that
cause va-sodilation (ie, expansion of the blood vessels). Examples include
exposure to an overly warm environment and ingestion of alco-hol or hot foods
and liquids. All can induce or intensify itching. Using a humidifier is helpful
if environmental air is dry. Activi-ties that result in perspiration should be
limited because perspi-ration may irritate and promote pruritus. If the patient
is troubled at night with itching that interferes with sleep, the nurse can
advise wearing cotton clothing next to the skin rather than synthetic
materials. The room should be kept cool and humidi-fied. Vigorous scratching
should be avoided, and nails kept trimmed to prevent skin damage and infection.
When the un-derlying cause of pruritus is unknown and further testing is
re-quired, the nurse explains each test and the expected outcome.
PERINEAL AND PERIANAL ITCHING
Pruritus
of the genital and anal regions may be caused by small particles of fecal
material lodged in the perianal crevices or attached to anal hairs or by
perianal skin damage caused by scratching, moisture, and decreased skin
resistance as a result of corticosteroid or antibiotic therapy. Other possible
causes of peri-anal itching include local irritants such as scabies and lice,
local lesions such as hemorrhoids, fungal or yeast infections, and pin-worm
infestation. Conditions such as diabetes mellitus, anemia, hyperthyroidism, and
pregnancy may also result in pruritus. Occasionally, no cause can be
identified.
Management
The
patient is instructed to follow proper hygiene measures and to discontinue home
and over-the-counter remedies. The per-ineal or anal area should be rinsed with
lukewarm water and blot-ted dry with cotton balls. Premoistened tissues may be
used after defecation. Cornstarch can be applied in the skinfold areas to
ab-sorb perspiration.
As
part of health teaching, the nurse instructs the patient to avoid bathing in
water that is too hot and to avoid using bubble baths, sodium bicarbonate, and
detergent soaps, all of which ag-gravate dryness. To keep the perineal or
perianal skin area as dry as possible, patients should avoid wearing underwear
made of synthetic fabrics. Local anesthetic agents should not be used be-cause
of possible allergic effects. The patient should also avoid vasodilating agents
or stimulants (eg, alcohol, caffeine) and me-chanical irritants such as rough
or woolen clothing. A diet that includes adequate fiber may help maintain soft
stools and prevent minor trauma to the anal mucosa.
Related Topics