Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Psoriasis - Noninfectious Inflammatory Dermatoses
Noninfectious Inflammatory
Dermatoses
PSORIASIS
Psoriasis is a chronic noninfectious inflammatory
disease of the skin in which epidermal cells are produced at a rate that is
about six to nine times faster than normal. The cells in the basal layer of the
skin divide too quickly, and the newly formed cells move so rapidly to the skin
surface that they become evident as profuse scales or plaques of epidermal
tissue. The psoriatic epidermal cell may travel from the basal cell layer of
the epidermis to the stratum corneum (ie, skin surface) and be cast off in 3 to
4 days, which is in sharp con-trast to the normal 26 to 28 days. As a result of
the increased num-ber of basal cells and rapid cell passage, the normal events
of cell maturation and growth cannot take place. This abnormal process does not
allow the normal protective layers of the skin to form.
One of the most common skin diseases, psoriasis
affects ap-proximately 2% of the population, appearing more often in people who
have a European ancestry. It is thought that the con-dition stems from a
hereditary defect that causes overproduction of keratin. Although the primary
cause is unknown, a combina-tion of specific genetic makeup and environmental
stimuli may trigger the onset of disease. There is some evidence that the cell
proliferation is mediated by the immune system. Periods of emo-tional stress
and anxiety aggravate the condition. Trauma, infec-tions, and seasonal and
hormonal changes also are trigger factors. The onset may occur at any age but
is most common between the ages of 15 and 50 years. Psoriasis has a tendency to
improve and then recur periodically throughout life (Champion et al., 1998).
Clinical Manifestations
Lesions appear as red, raised patches of skin
covered with silvery scales. The scaly patches are formed by the buildup of
living and dead skin resulting from the vast increase in the rate of skin-cell
growth and turnover (Fig. 56-4). If the scales are scraped away, the dark red
base of the lesion is exposed, producing multiple bleeding points. These
patches are not moist and may be pruritic. One variation of this condition is called
guttate psoriasis because the lesions remain about 1 cm wide and are scattered
like rain-drops over the body. This variation is believed to be associated with
a recent streptococcal throat infection. Psoriasis may range in severity from a
cosmetic source of annoyance to a physically disabling and disfiguring
disorder.
Particular sites of the body tend to be affected most by this condition; they include the scalp, the extensor surface of the el-bows and knees, the lower part of the back, and the genitalia. Bi-lateral symmetry is a feature of psoriasis. In approximately one fourth to one half of patients, the nails are involved, with pitting, discoloration, crumbling beneath the free edges, and separation of the nail plate. When psoriasis occurs on the palms and soles, it can cause pustular lesions called palmar pustular psoriasis.
Complications
The disease may be associated with asymmetric
rheumatoid factor– negative arthritis of multiple joints. The arthritic
development can occur before or after the skin lesions appear. The relation
between arthritis and psoriasis is not understood. Another complication is an
exfoliative psoriatic state in which the disease progresses to in-volve the
total body surface, called erythrodermic psoriasis. In this case, the patient
is more acutely ill, with fever, chills, and an elec-trolyte imbalance.
Erythrodermic psoriasis often appears in people with chronic psoriasis after
infections or after exposure to certain medications, including withdrawal of
systemic corticosteroids (Champion et al., 1998).
Assessment and Diagnostic Findings
The presence of the classic plaque-type lesions
generally confirms the diagnosis of psoriasis. Because the lesions tend to
change his-tologically as they progress from early to chronic plaques, biopsy
of the skin is of little diagnostic value. There are no specific blood tests
helpful in diagnosing the condition. When in doubt, the health professional
should assess for signs of nail and scalp involvement and for a positive
family history.
Medical Management
The goals of management are to slow the rapid
turnover of epi-dermis, to promote resolution of the psoriatic lesions, and to
con-trol the natural cycles of the disease. There is no known cure.
The therapeutic approach should be one that the
patient under-stands; it should be cosmetically acceptable and not too
disrup-tive of lifestyle. Treatment involves the commitment of time and effort
by the patient and possibly the family. First, any precipi-tating or aggravating
factors are addressed. An assessment is made of lifestyle, because psoriasis is
significantly affected by stress. The patient is informed that treatment of
severe psoriasis can be time consuming, expensive, and aesthetically
unappealing at times.
The
most important principle of psoriasis treatment is gen-tle removal of scales.
This can be accomplished with baths. Oils (eg, olive oil, mineral oil, Aveeno
Oilated Oatmeal Bath) or coal tar preparations (eg, Balnetar) can be added to
the bath water and a soft brush used to scrub the psoriatic plaques gently.
After bathing, the application of emollient creams containing alpha-hydroxy
acids (eg, Lac-Hydrin, Penederm) or salicylic acid will continue to soften
thick scales. The patient and family should be encouraged to establish a
regular skin care routine that can be maintained even when the psoriasis is not
in an acute stage.
PHARMACOLOGIC THERAPY
Three
types of therapy are standard: topical, intralesional, and systemic (Table
56-7).
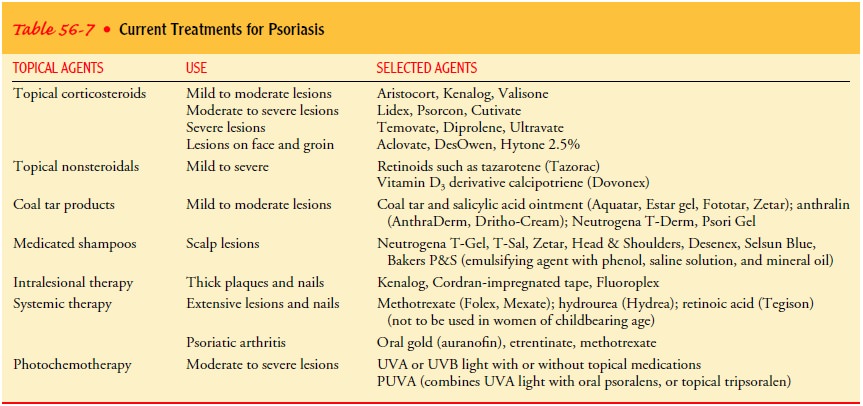
Topical Agents.
Topically applied agents are used to slow the overactive epidermis without affecting other tissues. Medications include tar preparations, anthralin, salicylic acid, and cortico-steroids. Two topical treatments introduced within the last few years are a vitamin D preparation, calcipotriene (Dovonex), and a retinoid compound, tazarotene (Tazorac). Treatment with these agents tends to suppress epidermopoiesis (ie, development of epidermal cells) and cause sloughing of the rapidly growing epi-dermal cells.
Topical formulations include lotions, ointments,
pastes, creams, and shampoos. Older treatments, including tar baths and
appli-cation of tar preparations on involved skin, are rarely used. Tar and
anthralin cause irritation of the skin at the sites of applica-tion, are
malodorous and difficult to apply, and do not give reli-able results. Newer
preparations that cause less irritation and have more consistent results are
becoming more widely used.
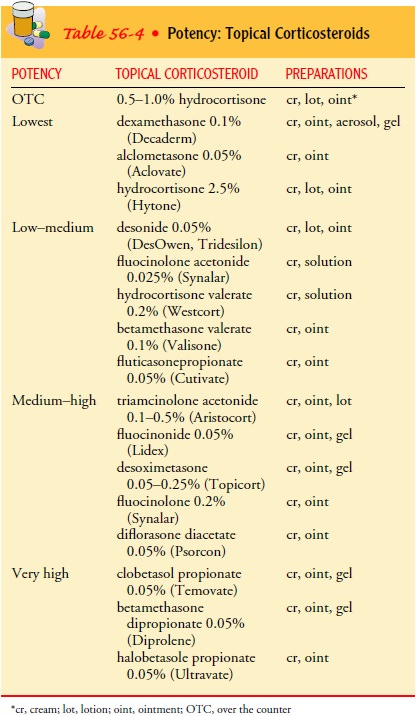
Topical
corticosteroids may be applied for their anti-inflammatory effect. Choosing the
correct strength of cortico-steroid for the involved site and choosing the most
effective vehicle base are important aspects of topical treatment. In general,
high-potency topical corticosteroids should not be used on the face and
intertriginous areas, and their use on other areas should be limited to a
4-week course of twice-daily applications. A 2-week break should be taken
before repeating treatment with the high-potency corticosteroids. For long-term
therapy, moderate-potency corti-costeroids are used. On the face and
intertriginous areas, only low-potency corticosteroids are appropriate for
long-term use (see Table 56-4).
Occlusive dressings may be applied to increase the
effective-ness of the corticosteroid. For the hospitalized patient, large
plas-tic bags may be used—one for the upper body with openings cut for the head
and arms and one for the lower body with openings for the legs. This leaves
only the extremities to wrap. In some der-matologic units, large rolls of
tubular plastic are used, such as those used by dry-cleaners. For patients
being treated at home, a vinyl jogging suit may be used. The medication is
applied, and the suit is put on over it. The hands can be wrapped in gloves,
the feet in plastic bags, and the head in a shower cap. Occlusive dress-ings
should not remain in place longer than 8 hours. The nurse should very carefully
inspect the skin for the appearance of atro-phy and telangiectasias which are
side effects of corticosteroids.
When
psoriasis involves large areas of the body, topical corti-costeroid treatment
can become expensive and involve some sys-temic risk. Some potent
corticosteroids, when applied to large areas of the body, have the potential to
cause adrenal suppression through percutaneous absorption of the medication. In
this event, other treatment modalities (eg, nonsteroidal topical med-ications,
ultraviolet light) may be used instead or in combination to decrease the need
for corticosteroids.
Newer nonsteroidal topical preparations are
available and ef-fective for many patients. Calcipotriene 0.05% (Dovonex) is a
derivative of vitamin D2. It works to decrease the mitotic turnover of the
psoriatic plaques. Its most common side effect is local irri-tation, and the
intertriginous areas and face should be avoided when using this medication.
Patients should be monitored for symptoms of hypercalcemia. It is available as
a cream for use on the body and a solution for the scalp. Calcipotriene is not
rec-ommended for use by elderly patients because of their more frag-ile skin or
for pregnant or lactating women.
The second advance in topical treatment of
psoriasis is tazarotene (Tazorac). Tazarotene, a retinoid, causes sloughing of
the scalescovering psoriatic plaques. As with other retinoids, it
causes in-creased sensitivity to sunlight, so patients should be cautioned to
use an effective sunscreen and avoid other photosensitizers (eg, tetracycline,
antihistamines). Tazarotene is listed as a Cate-gory X drug in pregnancy;
reports indicate evidence of fetal risk, and the risk of use in pregnant women
clearly outweighs any possible benefits. A negative result on a pregnancy test
should be obtained before initiating this medication, and an effective
contraceptive should be continued during treatment. Side effects of tazarotene
include burning, erythema, or irritation at the site of application and
worsening of psoriasis.
Intralesional Agents.
Intralesional injections of triamcinolone acetonide
(Aristocort, Kenalog-10, Trymex) can be administered directly into highly
visible or isolated patches of psoriasis that are resistant to other forms of
therapy. Care must be taken to ensure that normal skin is not injected with the
medication.
Systemic Agents.
Although systemic corticosteroids may cause rapid
improvement of psoriasis, their usual risks and the possi-bility of triggering
a severe flare-up on withdrawal limit their use. Systemic cytotoxic
preparations, such as methotrexate, have been used in treating extensive
psoriasis that fails to respond to other forms of therapy. Other systemic
medications in current use in-clude hydroxyurea (Hydrea) and cyclosporine A
(CyA).
Methotrexate
appears to inhibit DNA synthesis in epidermal cells, thereby reducing the
turnover time of the psoriatic epider-mis. However, the medication can be
toxic, especially to the liver, which can suffer irreversible damage.
Laboratory studies must be monitored to ensure that the hepatic, hematopoietic,
and renal systems are functioning adequately. Bone marrow suppression is another
potential side effect. The patient should avoid drinking alcohol while taking
methotrexate, because alcohol ingestion in-creases the possibility of liver
damage. The medication is terato-genic (ie, producing physical defects in the
fetus) and should not be administered to pregnant women.
Hydroxyurea
also inhibits cell replication by affecting DNA synthesis. The patient is
monitored for signs and symptoms of bone marrow depression.
Cyclosporine
A, a cyclic peptide used to prevent rejection of transplanted organs, has shown
some success in treating severe, therapy-resistant cases of psoriasis. Its use,
however, is limited by side effects such as hypertension and nephrotoxicity.
Oral
retinoids (ie, synthetic derivatives of vitamin A and its metabolite, vitamin A
acid) modulate the growth and differenti-ation of epithelial tissue. Etretinate
is especially useful for severe pustular or erythrodermic psoriasis. Etretinate
is a teratogen with a very long half-life; it cannot be used in women with
childbearing potential.
PHOTOCHEMOTHERAPY
One treatment for severely debilitating psoriasis
is a psoralen medication combined with ultraviolet-A (PUVA) light therapy.
Ultraviolet light is the portion of the electromagnetic spectrum containing
wavelengths ranging from 180 to 400 nm. In this treatment, the patient takes a
photosensitizing medication (usu-ally 8-methoxypsoralen) in a standard dose and
is subsequently exposed to long-wave ultraviolet light as the medication plasma
levels peak. Although the mechanism of action is not completely understood, it
is thought that when psoralen-treated skin is exposed to ultraviolet-A light,
the psoralen binds with DNA and decreases cellular proliferation. PUVA is not
without its hazards;it has been associated with long-term risks of skin cancer,
cataracts, and premature aging of the skin.
The
PUVA unit consists of a chamber that contains high-output black-light lamps and
an external reflectance system. The exposure time is calibrated according to
the specific unit in use and the anticipated tolerance of the patient’s skin.
The patient is usually treated two or three times each week until the psoriasis
clears. An interim period of 48 hours between treatments is nec-essary because
it takes this long for any burns resulting from PUVA therapy to become evident.
After
the psoriasis clears, the patient begins a maintenance program. Once little or
no disease is active, less potent therapies are used to keep minor flare-ups
under control.
Ultraviolet-B (UVB) light therapy is also used to
treat general-ized plaques. UVB light ranges from 270 to 350 nm, although
re-search has shown that a narrow range, 310 to 312 nm, is the action spectrum.
It is used alone or combined with topical coal tar. Side effects are similar to
those of PUVA therapy. A new development in light therapy is the narrow-band
UVB, which ranges from 311 to 312 nm, decreasing exposure to harmful
ultraviolet energy while providing more intense, specific therapy (Shelk &
Morgan, 2000).
If access to a light treatment unit is not
feasible, the patient can expose himself or herself to sunlight. The risks of
all light treatments are similar and include acute sunburn reaction;
exac-erbation of photosensitive disorders such as lupus, rosacea, and
polymorphic light eruption; and other skin changes such as in-creased wrinkles,
thickening, and an increased risk for skin cancer.
Excimer
lasers have come into use in treating psoriasis. These lasers function at 308
nm. Studies show that medium-sized pso-riatic plaques clear in four to six
treatments and remain clear for up to 9 months. A laser can be more effective
on the scalp or on other hard-to-treat areas, because the laser can be aimed
very specifically on the plaque (Lebwohl, 2000). Table 56-7 summa-rizes the
treatment plans.
Related Topics