Chapter: Medical Surgical Nursing: Management of Patients With Dermatologic Problems
Fungal (Mycotic) Infections
Fungal (Mycotic) Infections
Fungi,
tiny members of a subdivision of the plant kingdom that feed on organic matter,
are responsible for various common skin infections. In some cases, they affect
only the skin and its ap-pendages (ie, hair and nails). In other cases, the
internal organs are involved, and this disease may be life-threatening.
Superficial infections, however, rarely cause even temporary disability and
respond readily to treatment. Secondary infection with bacteria, Candida, or both organisms may occur.
The
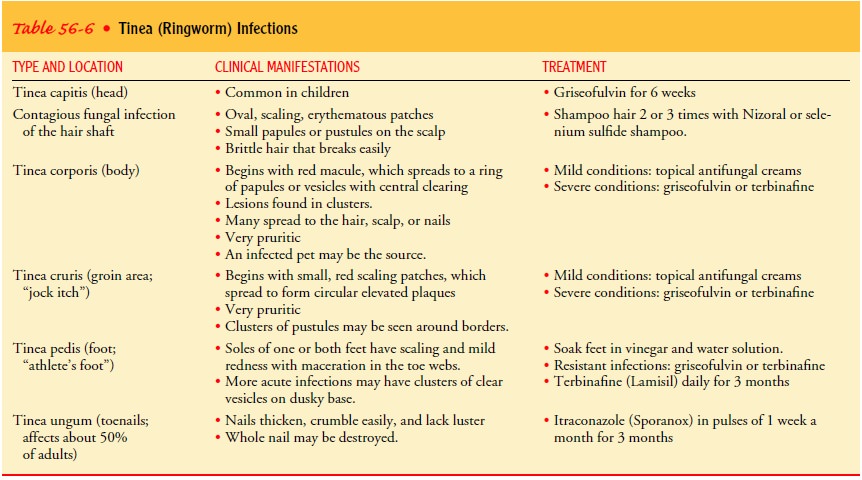
most common fungal skin infection is tinea,
which is also called ringworm because of its characteristic appearance of ring
or rounded tunnel under the skin. Tinea infections affect the head, body,
groin, feet, and nails. Table 56-6 summarizes the tinea in-fections.
To
obtain a specimen for diagnosis, the lesion is cleaned, and a scalpel or glass
slide is used to remove scales from the margin of the lesion. The scales are
dropped onto a slide to which potassium hydroxide has been added. The diagnosis
is made by examination of the infected scales microscopically for spores and
hyphae or by isolating the organism in culture. Under Wood’s light, a speci-men
of infected hair appears fluorescent; this may be helpful in diagnosing some
cases of tinea capitis.
TINEA PEDIS: ATHLETE’S FOOT
Tinea
pedis (ie, athlete’s foot) is the most common fungal infec-tion. It is
especially prevalent in those who use communal show-ers or swimming pools (Odom
et al., 2000).
Clinical Manifestations
Tinea
pedis may appear as an acute or chronic infection on the soles of the feet or
between the toes. The toenail may also be involved. Lymphangitis and cellulitis
occur occasionally when bacterial superinfection occurs. Sometimes, a mixed
infection in-volving fungi, bacteria, and yeast occurs.
Medical Management
During
the acute, vesicular phase, soaks of Burow’s solution or potassium permanganate
solutions are used to remove the crusts, scales, and debris and to reduce the
inflammation. Topical anti-fungal agents (eg, miconazole, clotrimazole) are
applied to the in-fected areas. Topical therapy is continued for several weeks
because of the high rate of recurrence.
Nursing Management
Footwear provides a favorable environment for fungi, and the causative fungus may be in the shoes or socks. Because moisture encourages the growth of fungi, the patient is instructed to keep the feet as dry as possible, including the areas between the toes.
Small pieces of cotton can be placed between the
toes at night to absorb moisture. Socks should be made of cotton, and hosiery
should have cotton feet, because cotton is an effective absorber of
perspiration.
For
people whose feet perspire excessively, perforated shoes permit better aeration
of the feet. Plastic- or rubber-soled footwear should be avoided. Talcum powder
or antifungal powder applied twice daily helps to keep the feet dry. Several
pairs of shoes should be alternated so that they can dry completely before
being worn again.
TINEA CORPORIS:RINGWORM OF THE BODY
In
tinea corporis (ie, ringworm of the body), the typical ringed le-sion appears
on the face, neck, trunk, and extremities (Fig. 56-3). Animal (nonhuman)
varieties are known to cause an intense in-flammatory reaction in humans
because they are not adapted to living on human hosts. Humans make contact with
animal va-rieties through contact with pets or objects that have been in
contact with an animal.

Medical Management
Topical antifungal medication may be applied to
small areas. Oral antifungal agents are used only in extensive cases. Side
ef-fects of oral antifungal agents include photosensitivity, skin rashes,
headache, and nausea. Newer antifungal agents, including itra-conazole,
fluconazole, and terbinafine, have been more effective with fewer systemic side
effects than griseofulvin in patients with chronic fungal (dermatophyte)
infections.
Nursing Management
The
patient is instructed to use a clean towel and washcloth daily. Because fungal
infections thrive in heat and moisture, all skin areas and skin folds that
retain moisture must be dried thor-oughly. Clean cotton clothing should be worn
next to the skin.
TINEA CAPITIS:RINGWORM OF THE SCALP
Ringworm of the scalp is a contagious fungal infection of the hair shafts and a common cause of hair loss in children. Any child with scaling of the scalp should be considered to have tinea capi-tis until proven otherwise. Clinical examination reveals one or several round, red scaling patches. Small pustules or papules may be seen at the edges of such patches.
As the hairs in the affected areas are
invaded by the fungi, they become brittle and break off at or near the surface
of the scalp, leaving bald patches or the clas-sic sign of black dots, which
are the broken ends of hairs. Because most cases of tinea capitis heal without
scarring, the hair loss is only temporary.
Medical Management
Griseofulvin, an antifungal agent, is prescribed
for patients with tinea capitis. Topical agents do not provide an effective
cure be-cause the infection occurs within the hair shaft and below the surface
of the scalp. However, topical agents can be used to in-activate organisms
already on the hair. This minimizes contagion and eliminates the need to clip
the hair. Infected hairs break off anyway, and noninfected ones may remain in
place. The hair should be shampooed two or three times weekly, and a topical
anti-fungal preparation should be applied to reduce dissemination of the
organisms.
Nursing Management
Because tinea capitis is contagious, the patient
and family should be instructed to set up a hygiene regimen for home use. Each
per-son should have a separate comb and brush and should avoid ex-changing hats
and other headgear. All infected members of the family must be examined because
familial infections are relatively common. Household pets should also be
examined.
TINEA CRURIS:RINGWORM OF THE GROIN
Tinea
cruris (ie, jock itch) is ringworm infection of the groin, which may extend to
the inner thighs and buttock area. It occurs most frequently in young joggers,
obese people, and those who wear tight underclothing. The incidence of tinea
cruris is in-creased among people with diabetes.
Management
Mild
infections may be treated with topical medication such as clotrimazole,
miconazole, or terbinafine for at least 3 to 4 weeks to ensure eradication of
the infection. Oral antifungal agents may be required for more severe
infections. Heat, friction, and mac-eration (from sweating) predispose the
patient to the infection. The nurse instructs the patient to avoid excessive
heat and hu-midity as much as possible and to avoid wearing nylon under-wear,
tight-fitting clothing, and a wet bathing suit. The groin area should be
cleaned, dried thoroughly, and dusted with a topical antifungal agent such as
tolnaftate (Tinactin) as a preventive mea-sure, because the infection is likely
to recur.
TINEA UNGUIUM: ONYCHOMYCOSIS
Tinea
unguium (ie, ringworm of the nails) is a chronic fungal in-fection of the
toenails or, less commonly, the fingernails. It is usu-ally caused by Trichophyton species (T. rubrum, T. mentagrophytes) or Candida albicans. It is usually
associated with long-standing fungal infection of the feet. The nails become
thickened, friable (ie, easily crumbled), and lusterless. In time, debris
accumulates under the free edge of the nail. Ultimately, the nail plate
separates. Because of the chronicity of this infection, the entire nail may be
destroyed.
Management
An oral antifungal agent is prescribed for 6 weeks
when the fin-gernails are involved and 12 weeks when the toenails are involved.
Selection of the antifungal agent depends on the causative fun-gus. Candidal
infections are treated with fluconazole (Diflucan) or itraconazole (Sporanox).
Griseofulvin is no longer considered effective therapy because of its long
treatment course and poor cure rate. Response to oral antifungal agents in treating
infections of the toenails is poor at best. Frequently, when the treatment
stops, the infection returns.
Related Topics