Chapter: Clinical Anesthesiology: Anesthetic Management: Cardiovascular Physiology & Anesthesia
Systemic Circulation
Systemic Circulation
The systemic vasculature can be divided
function-ally into arteries, arterioles, capillaries, and veins. Arteries are
the high-pressure conduits that supply the various organs. Arterioles are the
small vessels that directly feed and control blood flow through each capillary
bed. Capillaries are thin-walled ves-sels that allow the exchange of nutrients
between blood and tissues. Veins return blood from capillary beds to the heart.
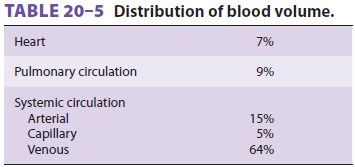
The distribution of blood between the
various components of the circulatory system is shown in Table 20–5. Note that most of
the blood volumeis in the systemic circulation—specifically, within systemic
veins. Changes in systemic venous tone allow these vessels to function as a
reservoir for blood. Following significant blood or fluid losses, a
sympathetically mediated increase in venous tone reduces the caliber of these
vessels and shifts blood into other parts of the vascular system. Conversely,
venodilation allows these vessels to accommodate increases in blood volume.
Sympathetic control of venous tone is an important determinant of venous
return to the heart. Reduced venous tone
following induction of anesthesia frequently results in venous pooling of blood
and contributes to hypotension.
A multiplicity of factors influences blood flow in the vascular tree. These include mechanisms of local and metabolic control, endothelium-derived factors, the autonomic nervous system, and circulat-ing hormones.
AUTOREGULATION
Most tissue beds regulate their own
blood flow (autoregulation). Arterioles generally dilate in response to reduced
perfusion pressure or increased tissue demand. Conversely, arterioles constrict
in response to increased pressure or reduced tissue demand. These phenomena are
likely due to both an intrinsic response of vascular smooth muscle to stretch
and the accumulation of vasodilatory met-abolic by-products. The latter may
include K+, H+, CO2, adenosine, and lactate.
ENDOTHELIUM DERIVED FACTORS
The vascular endothelium is
metabolically active in elaborating or modifying substances that directly or
indirectly play a major role in controlling blood pressure and flow. These
include vasodilators (eg, nitric oxide, prostacyclin [PGI2]), vasoconstrictors (eg, endothelins, thromboxane A2), anticoagulants (eg, thrombomodulin, protein C),
fibrinolytics (eg, tissue plasminogen activator), and factors that inhibit
platelet aggregation (eg, nitric oxide and PGI2).
Nitric oxide is synthesized from arginine by nitric oxide synthetase. This
substance has a number of func-tions In the circulation, it is a potent
vasodilator. It binds guanylate cyclase, increasing cGMP levels and producing
vasodilation. Endothelially derived vaso-constrictors (endothelins) are
released in response to thrombin and epinephrine.
Related Topics