Chapter: Clinical Anesthesiology: Anesthetic Management: Cardiovascular Physiology & Anesthesia
Assessment of Ventricular Function
ASSESSMENT OF VENTRICULAR FUNCTION
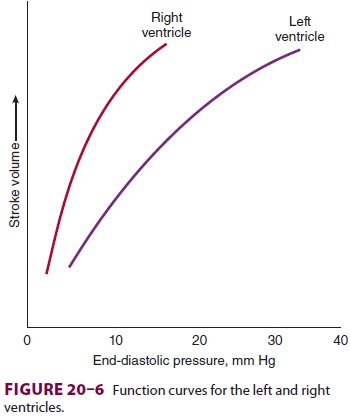
1. Ventricular Function Curves
Plotting cardiac output or stroke volume
against preload is useful in evaluating pathological states and understanding
drug therapy. Normal right and left ventricular function curves are shown in Figure 20–6.
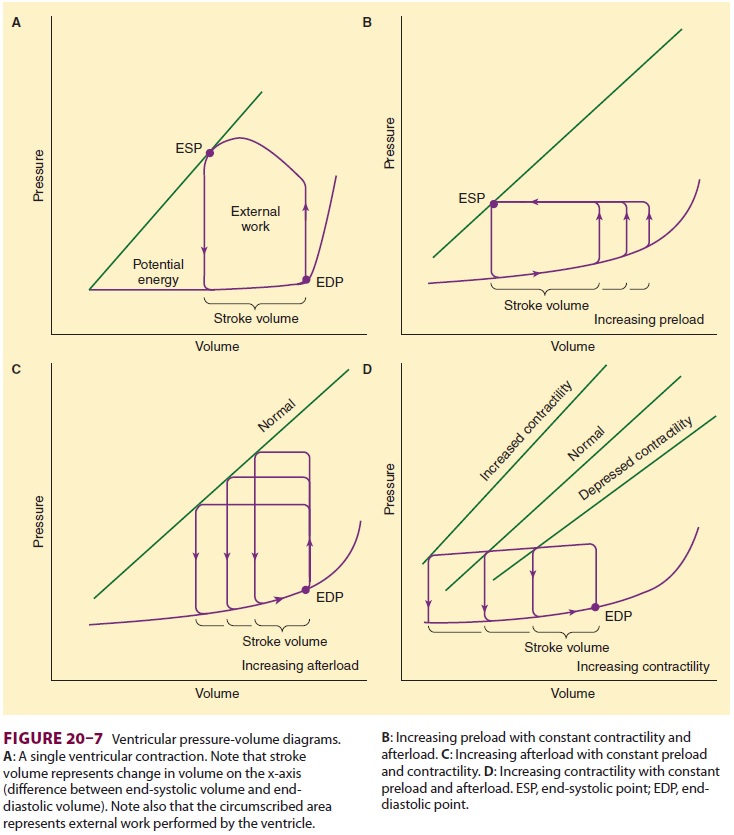
Ventricular pressure–volume diagrams are
use-ful because they dissociate contractility from both preload and afterload.
Two points are identified on such diagrams: the end-systolic point (ESP) and
the end-diastolic point (EDP) (Figure 20–7). ESP is reflective of systolic
function, whereas EDP is more reflective of diastolic function. For any given
con-tractile state, all ESPs are on the same line (ie, the relationship between
end-systolic volume and end-systolic pressure is fixed).
2. Assessment of Systolic Function
The change in ventricular pressure over time dur-ing systole (dP/dt) is defined by the first derivative of the ventricular pressure curve and is often used as a measure of contractility. Contractility is directly proportional to dP/dt, but accurate measurement of this value requires a high-fidelity (“Millar”) ven-tricular catheter; however, it can be estimated with echocardiography. Although arterial pressure trac-ings are distorted due to properties of the vascular tree, the initial rate of rise in pressure (the slope) can serve as a rough approximation; the more proxi-mally the arterial line catheter is located in the arte-rial tree, the more accurate the extrapolation will be. The usefulness of dP/dt is also limited in that it may be affected by preload, afterload, and heart rate.
Ejection Fraction
The ventricular ejection fraction (EF),
the fraction of the end-diastolic ventricular volume ejected, is the most
commonly used clinical measurement of systolic function. EF can be calcu-lated
by the following equation:
where EDV is left ventricular diastolic
volume and ESV is end-systolic volume. Normal EF is
approximately 0.67 ± 0.08. Measurements can be made preoperatively from
cardiac catheterization, radionucleotide studies, or transthoracic (TTE) or
transesophageal echocardiography (TEE).Pulmonary artery catheters with
fast-response thermistors allow measurement of the right ventric-ular EF.
Unfortunately, when pulmonary vascular resistance increases, decreases in right
ventricular
EF may reflect afterload rather than
contractility. Left ventricular EF is not an accurate measure of ventricular
contractility in the presence of mitral insufficiency.
3. Assessment of Diastolic Function
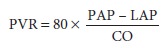
Left ventricular diastolic function can
be assessed clinically by Doppler echocardiography on a transthoracic or
transesophageal examination. Flow velocities are measured across the mitral
valve during diastole. Three patterns of diastolic dysfunction are generally
recognized based on isovolumetric relaxation time, the ratio of peak early
diastolic flow (E) to peak atrial sys-tolic flow (A), and the deceleration time
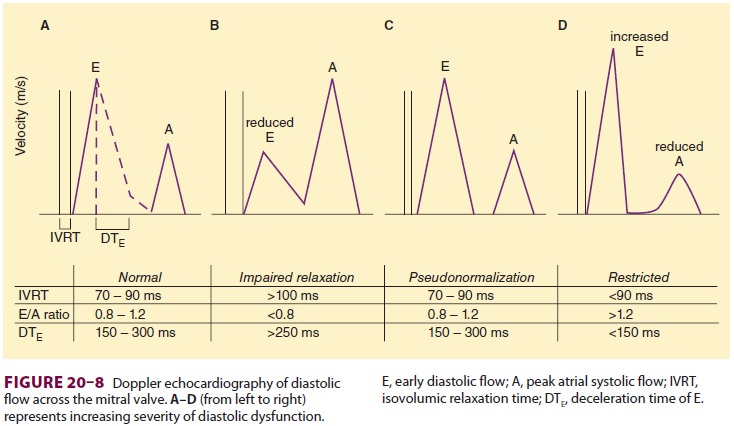
(DT) of E (DTE) (Figure 20–8). Tissue Doppler is frequently
used to distinguish “pseudonormal” from normal diastolic function. Tissue
Doppler is also an excel-lent way to detect “conventional” diastolic dysfunc-tion.
An e’ wave peak velocity of less than 8 cm/sec is associated with impaired
diastolic function. An E/e’ wave ratio that is greater than 15 is consistent
with elevated left ventricular end-diastolic pressure (Figure 20–9).
Related Topics