Chapter: Clinical Anesthesiology: Anesthetic Management: Cardiovascular Physiology & Anesthesia
Arterial Blood Pressure
ARTERIAL BLOOD PRESSURE
Systemic blood flow is pulsatile in
large arteries because of the heart’s cyclic activity; by the time blood
reaches the systemic capillaries, flow is con-tinuous (laminar). The mean
pressure falls to less than 20 mm Hg in the large systemic veins that return
blood to the heart. The largest pressure drop, nearly 50%, is across the arterioles,
and the arterioles account for the majority of SVR.MAP is proportionate to the
product of SVR × CO. This relationship is based on an analogy to Ohm’s law, as
applied to the circulation:
MAP − CVP ≈ SVR × CO
Because CVP is normally very small
compared with MAP, the former can usually be ignored. From this relationship,
it is readily apparent that hypo-tension is the result of a decrease in SVR,
CO, or both: To maintain arterial blood pressure, a decrease in either SVR or
CO must be compensated by an increase in the other. MAP can be measured as the
integrated mean of the arterial pressure waveform.Alternatively, MAP may be
estimated by the follow-ing formula:
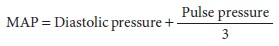
where pulse pressure is the difference
between sys-tolic and diastolic blood pressure. Arterial pulse pressure is
directly related to stroke volume, but is inversely proportional to the
compliance of the arte-rial tree. Thus, decreases in pulse pressure may be due
to a decrease in stroke volume, an increase in SVR, or both. Increased pulse
pressure increases shear stress on vessel walls, potentially leading to
atherosclerotic plaque rupture and thrombosis or rupture of aneurysms.
Increased pulse pressure in patients undergoing cardiac surgery has been
associ-ated with adverse renal and neurological outcomes.
Transmission of the arterial pressure
wave from large arteries to smaller vessels in the periphery is faster than the
actual movement of blood; the pres-sure wave velocity is 15 times the velocity
of blood in the aorta. Moreover, reflections of the propagating waves off
arterial walls widen pulse pressure before the pulse wave is completely
dampened in very small arteries.
Control of Arterial Blood Pressure
Arterial blood pressure is regulated by
a series of immediate, intermediate, and long-term adjust-ments that involve
complex neural, humoral, and renal mechanisms.
A. Immediate Control
Minute-to-minute control of blood
pressure is pri-marily the function of autonomic nervous system reflexes.
Changes in blood pressure are sensed both centrally (in hypothalamic and
brainstem areas) and peripherally by specialized sensors (barorecep-tors).
Decreases in arterial blood pressure result in increased sympathetic tone,
increased adrenal secre-tion of epinephrine, and reduced vagal activity. Theresulting systemic vasoconstriction,
increased heart rate, and enhanced cardiac contractility serve to increase
blood pressure.
Peripheral baroreceptors are located at
the bifurcation of the common carotid arteries and the aortic arch. Elevations
in blood pressure increasebaroreceptor discharge, inhibiting systemic
vaso-constriction and enhancing vagal tone (barorecep-tor
reflex). Reductions in blood pressure decreasebaroreceptor discharge,
allowing vasoconstriction and reduction of vagal tone. Carotid baroreceptors
send afferent signals to circulatory brainstem centers via Hering’s nerve (a
branch of the glossopharyngeal nerve), whereas aortic baroreceptor afferent
signals travel along the vagus nerve. Of the two peripheral sensors, the carotid
baroreceptor is physiologi-cally more important and is primarily responsible
for minimizing changes in blood pressure that are caused by acute events, such
as a change in posture. Carotid baroreceptors sense MAP most effectively
between pressures of 80 and 160 mm Hg. Adapta-tion to acute changes in blood
pressure occurs over the course of 1–2 days, rendering this reflex inef-fective
for longer term blood pressure control. All volatile anesthetics depress the
normal barorecep-tor response, but isoflurane and desflurane seem to have less
effect. Cardiopulmonary stretch receptors located in the atria, left ventricle,
and pulmonary circulation can cause a similar effect.
B. Intermediate Control
In the course of a few minutes,
sustained decreases in arterial pressure, together with enhanced sym-pathetic
outflow, activate the renin–angiotensin– aldosterone system, increase secretion
of arginine vasopressin (AVP), and alter normal capillary fluid exchange. Both
angiotensin II and AVP are potent arteriolar vasoconstrictors. Their immedi-ate
action is to increase SVR. In contrast to forma-tion of angiotensin II, which
responds to relatively smaller changes, sufficient AVP secretion to pro-duce
vasoconstriction will only occur in response to more marked degrees of
hypotension. Angiotensin constricts arterioles via AT 1 receptors. AVP medi-ates vasoconstriction via V 1 receptors and exerts its antidiuretic effect via V 2 receptors.
Sustained changes in arterial blood
pressure can also alter fluid exchange in tissues by their sec-ondary effects
on capillary pressures. Hypertension increases interstitial movement of
intravascular fluid, whereas hypotension increases reabsorption of interstitial
fluid. Such compensatory changes in intravascular volume can reduce fluctuations
in blood pressure, particularly in the absence of ade-quate renal function .
C. Long-Term Control
The effects of slower renal mechanisms
become apparent within hours of sustained changes in arte-rial pressure. As a
result, the kidneys alter total body sodium and water balance to restore blood
pres-sure to normal. Hypotension results in sodium (and water) retention,
whereas hypertension generally increases sodium excretion in normal
individuals.
Related Topics