Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Critical Care
Septic Shock
SEPTIC SHOCK
The SCCM/ESICM/ACCP/ATS/SIS Consensus
Conference defined septic shock as sepsis asso-ciated
with hypotension (systolic blood pressure <90 mm Hg, mean arterial pressure <60 mm Hg, or systemic
blood pressure <40 mm Hg from baseline) despite adequate fluid resuscitation. Septic
shock is usually characterized by inadequate tissue perfusion and widespread
cellular dysfunction. In contrast to other forms of shock (hypovolemic,
cardiogenic, neurogenic, or anaphylactic), cellular dysfunction in septic shock
is not necessarily related to the hypo-perfusion. Instead, metabolic blocks at
the cellu-lar and microcirculation levels may contribute to impaired cellular
oxidation.
Pathophysiology
An infectious process that induces a severe
or pro-tracted SIRS can result in septic shock. In hospital-ized patients
septic shock most commonly follows gram-negative infections in either the
genitourinary tract or the lungs, but identical presentations can be seen with
other pathogens. In up to 50% of cases of severe sepsis no organisms can be
cultured from blood. Hypotension is due to a decreased circulating
intravascular volume resulting from a diffuse capil-lary leak. Patients may
also have myocardial depres-sion. Activation of platelets and the coagulation
cascade can lead to the formation of fibrin-platelet aggregates, which further
compromise tissue blood flow. Hypoxemia from ARDS accentuates tissue hypoxia.
The release of vasoactive substances and formation of microthrombi in the
pulmonary circu-lation increase pulmonary vascular resistance.
Hemodynamic Subsets
The circulation in patients with septic shock
is often described as either hyperdynamic or hypodynamic. In reality, both
represent the same process, but their expression depends on preexisting cardiac
function and intravascular volume and the patient’s response. Systemic
venodilation and transudation of fluid into tissues result in relative hypovolemia
in patients with sepsis. Hyperdynamic septic
shock is characterized by normal or elevated cardiac out-put and profoundly
reduced systemic vascular resis-tance. Decreased myocardial contractility is
often demonstrable by echocardiography even in hyper-dynamic patients with
increased cardiac output. Mixed venous oxygen saturation is characteristically
increased in the absence of hypoxemia and likely reflects the increased cardiac
output and the cellular metabolic defect in oxygen utilization.
It used to be accepted wisdom that
hypody-namic septic shock, characterized by decreased car-diac output with low
or normal systemic vascular resistance, was usually seen later in the course of
shock. This view is false; hypodynamic shock often occurs early in the course
of septic shock. It is more likely to be seen in severely hypovolemic patients
and in those with underlying cardiac disease. Myo-cardial depression is
prominent. Mixed venous oxygen saturation is reduced in these patients, and
pulmonary hypertension is often prominent. Eleva-tion of pulmonary vascular
resistance widens the normal pulmonary artery diastolic-to-wedge pres-sure
gradient; large gradients have been associated with a higher mortality rate.
The increase in pulmo-nary vascular resistance may contribute to right
ven-tricular dysfunction.
Clinical Manifestations
Manifestations of septic shock appear to be pri-marily related to host
response rather than the infective agent. Septic shock classically presents
with an abrupt onset of chills, fever, nausea (and often vomiting), decreased
mental status, tachy-pnea, hypotension, and tachycardia. The patient may appear
flushed and feel warm (hyperdynamic) or pale with cool and often cyanotic
extremities (hypodynamic). In old, debilitated patients and in infants, the
diagnosis often is less obvious and hypothermia may be seen.
Leukocytosis with a leftward shift to
premature cell forms is typical, but leukopenia can be seen with overwhelming
sepsis and is an ominous sign. Pro-gressive metabolic acidosis (usually lactic
acidosis) is typically partially compensated by a concomitant respiratory
alkalosis. Elevated lactate levels reflect both increased production resulting
from poor tis-sue perfusion and decreased uptake by the liver and kidneys.
Hypoxemia may herald the onset of ARDS. Oliguria due to the combination of
hypovolemia, hypotension, and a systemic inflammatory insult will often
progress to kidney failure. Elevations in serum aminotransferases and bilirubin
are due to hepatic dysfunction. Insulin resistance is uniformly present and
produces hyperglycemia. Thrombocyto-penia is common and is often an early sign
of sepsis. Laboratory evidence of disseminated intravascular coagulation (DIC)
is often present but is rarely asso-ciated with a bleeding diathesis. The
latter responds only to control of the sepsis. Stress ulceration of gas-tric
mucosa is common. Respiratory and kidney fail-ure are the leading causes of
death in septic patients.
Neutropenic patients (absolute neutrophil count 500/µL) may develop macular or papular
lesions that can ulcerate and become gangrenous (ecthyma gangrenosum). These
lesions are com-monly associated with Pseudomonas
septicemia but can be caused by other organisms. Perirectal abscesses can
develop very quickly in neutropenic patients with few external signs; conscious
patients may complain only of perirectal pain.
Treatment
Septic shock is a medical emergency that requires immediate
intervention. Treatment is threefold:
control and eradication of the infection by
appro-priate and timely intravenous antibiotics, drainage of abscesses,
debridement of necrotic tissues, and removal of infected foreign bodies; (2)
maintenance of adequate perfusion with intravenous fluids and inotropic and
vasopressor agents; and (3) supportive treatment of complications such as ARDS,
kidney failure, gastrointestinal bleeding, and DIC.
Antibiotic treatment usually is initiated
before pathogens are identified but only after adequate cul-tures are obtained
(commonly, blood, urine, wounds, and sputum). Pending the results of cultures
and tests of antibiotic sensitivity, combination therapy with two or more
antibiotics is generally indicated. Typi-cally, the combination of a
penicillin/β-lactamase inhibitor or
third-generation cephalosporin with an aminoglycoside is used. The choice
depends on which organisms are seen with the greatest frequency in one’s
medical center. Additional diagnostic stud-ies may be indicated (eg,
thoracentesis, paracentesis, lumbar puncture, or imaging), depending on the
history and physical examination.
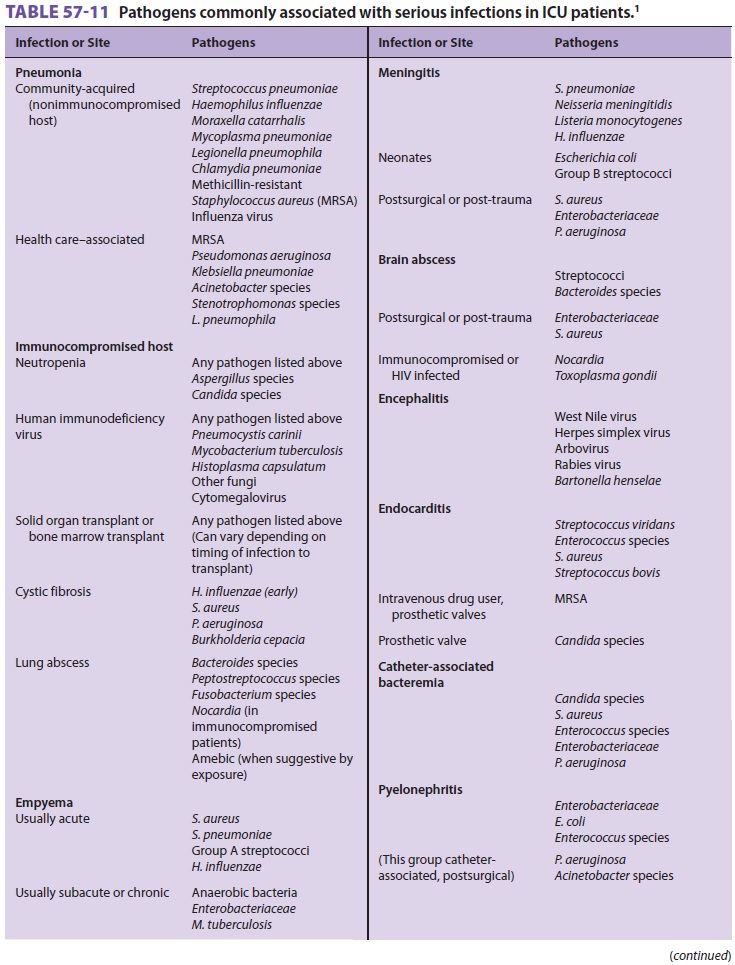
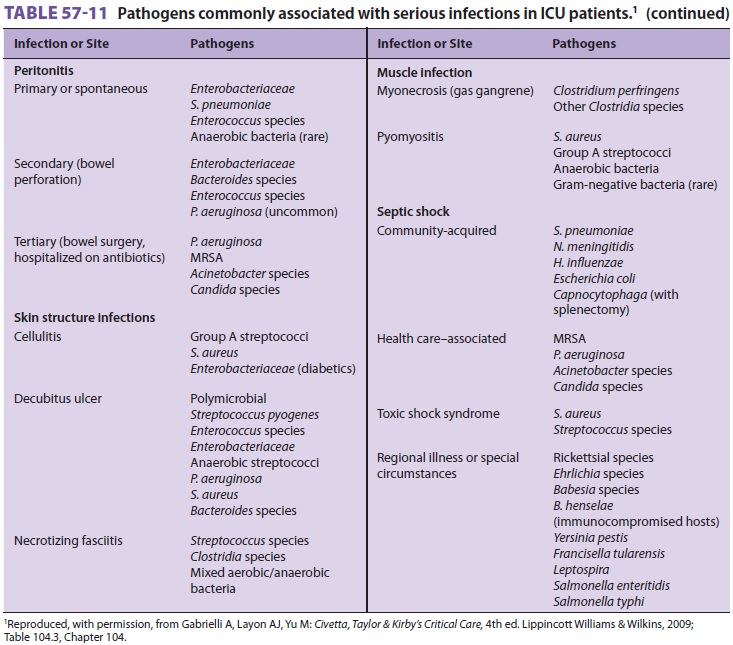
Empiric antibiotic therapy in
immunocompro-mised patients should be based on pathogens that are generally
associated with the immune defect (see Table 57–11). Vancomycin is added if
intravascular catheter-related infection is suspected. Clindamy-cin or
metronidazole may be given to neutrope-nic patients if a rectal abscess is
suspected. Many clinicians initiate therapy for a presumed fungal infection
when an immunocompromised patient continues to experience fever despite
antibiotic therapy. Granulocyte colony-stimulating factor or
granulocyte–macrophage colony-stimulating factor may be used to shorten the
period of neutropenia; granulocyte transfusion may occasionally be used in
refractory gram-negative bacteremia. Diffuse interstitial infiltrates on a
chest radiograph may sug-gest unusual bacterial, parasitic, or viral pathogens;
many clinicians initiate empiric therapy with trim-ethoprim-sulfamethoxazole
and erythromycin in such instances. Nodular infiltrates on a radiograph suggest
a fungal pneumonia and may warrant anti-fungal therapy. Antiviral therapy
should be consid-ered in septic patients who are more than 1 month post–bone
marrow or solid organ transplantation.
In general, therapy should follow the most
recent SCCM/ESICM “surviving sepsis” guidelines. The presence of inadequate
perfusion is determined by measurement of blood lactate. “Goal-directed”
hemodynamic support is also recommended by many groups. Tissue oxygenation and
perfusion are supported with oxygen, intravenous fluids, inotro-pes, and
vasopressors. Central venous pressure is maintained at greater than 8 mm Hg and
central venous oxygen saturation is maintained at greater than 70%. Packed red
blood cell transfusions are given to keep hemoglobin levels greater than 8 g/dL,
especially when central venous pressure and cen-tral venous oxygen saturation
are below targets. Marked “third-spacing” has long been regarded as
characteristic of septic shock, but currently there is debate regarding the
existence of the third space and the administration of large volumes of
intravenous fluid as to which is cause and which is effect. Colloid solutions
more rapidly restore intravascular volume compared with crystalloid solutions
but other-wise offer no proven additional benefit. Vasopres-sor therapy is generally initiated if
hypotension (mean arterial pressure <65 mm Hg) or elevated blood lactate levels persist following
administra-tion of intravenous
fluids. Suggested choices arenorepinephrine or
dopamine; other positive ino-tropic drugs (eg, dobutamine) are indicated only
when the SVO2 falls below 70% despite fluids and vasopressor therapy. Patients with
persisting eleva-tions of lactate or persisting low central venous oxy-gen
saturations, despite treatment, should receive a week-long course of steroids
(200–300 mg/d of hydrocortisone or the equivalent in divided doses or by
infusion). Blood glucose should be controlled with a target value of less than
180 mg/dL. In patients with hypotension that is refractory to norepineph-rine
plus dopamine or dobutamine, vasopressin may be administered to improve blood
pressure. Severe acidosis may decrease the efficacy of inotropes and should
therefore generally be corrected (pH > 7.20) with bicarbonate or THAM infusion in
patients with refractory hypotension and lactic acidosis. “Renal” doses of
dopamine or fenoldopam may increase uri-nary output but have not been shown to
improve or protect kidney function or patient outcomes. Clinical trials of
naloxone, opsonins (fibronectin), inhibitors of the coagulation cascade
(drotrecogin alfa), and monoclonal antibodies directed against
lipopolysaccharide in septic shock have been disappointing.
Related Topics