Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Critical Care
Increased Permeability Pulmonary Edema (Noncardiogenic Pulmonary Edema): Acute Lung Injury & ARDS
Increased
Permeability Pulmonary Edema (Noncardiogenic Pulmonary Edema): Acute Lung
Injury & ARDS
Extravascular lung water increases in
patients with increased permeability pulmonary edema due to enhanced
permeability or disruption of the capillary–alveolar membrane. The protective
effect of plasma oncotic pressure is lost as increased amounts of albumin
“leak” into the pulmonary inter-stitium; normal—or even low—capillary
hydrostatic pressures are unopposed and result in transudation of fluid into
the lungs. Permeability edema is seen with acute lung injury (P:F ratio ≤ 300 [P = PaO2 and F = FIO2]) and is often associated with sepsis, trauma, and pulmonary
aspiration; when severe (P:F ratio < 200), it is referred to as the acute
respiratory distress syndrome (ARDS).
Pathophysiology
Acute lung injury and ARDS represent the
pul-monary manifestation of the systemic inflamma-tory response syndrome
(SIRS). Central to the pathophysiology of acute lung injury and ARDS is severe
injury of the capillary–alveolar membrane. Regardless of the type of injury,
the lung responds to the ensuing inflammatory response in a similar fashion.
The released secondary mediators increase pulmonary capillary permeability,
induce pulmo-nary vasoconstriction, and alter vascular reactivity such that hypoxic
pulmonary vasoconstriction is abolished. Destruction of alveolar epithelial
cells is prominent. Alveolar flooding, with decreased surfactant production
(due to loss of type II pneu-mocytes), result in collapse. The exudative phase
of ARDS may persist for a varying period; it is often followed by a fibrotic
phase (fibrosing alveolitis), which in some cases leads to permanent scarring.
Clinical Manifestations
The diagnosis of acute lung injury or ARDS requires the exclusion of
significant underlying left ventric-ular dysfunction combined with a P:F ratio
of less than 300 (acute lung injury) or less than 200 (ARDS), and the presence
of diffuse infiltrates on chest radio-graph. The lung is often affected in a
nonhomoge-neous pattern, although dependent areas tend to be most affected.
Acute lung injury and ARDS are commonly seen in the settings of sepsis
or trauma. Patients present with severe dyspnea and labored respira-tions.
Hypoxemia due to intrapulmonary shunting is a universal finding. Although dead
space venti-lation is increased, arterial CO2 tension is typically decreased
because of a marked increase in minute ventilation. Ventilatory failure may be
seen initially in severe cases or may eventually develop due to respiratory
muscle fatigue or marked destruction of the capillary–alveolar membrane.
Pulmonary hypertension and low or normal left ventricular filling pressures are
characteristic hemodynamic findings.
Treatment
In
addition to intensive respiratory care, treatment should be directed at reversible
processes such as sepsis or hypotension. Hypoxemia is treated with oxygen
therapy. Milder cases may be treated with a CPAP mask, but most patients
require intubation and at least some degree of mechanical ventilatory support.
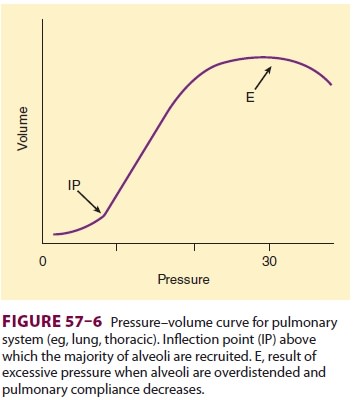
Increased Pplt pressures (>30 cm H 2O) and high VT (>6 mL/kg), however,
should also be avoided because overdistention of alveoli can induce iatrogenic
lung injury, as can high FIO2(>0.5).
While injury from high FIO2hasnot been conclusively
demonstrated inhumans, as was previously noted, VT of 12 mL/kg was associated
with greater mortality than VT of6 mL/kg and Pplt of less than 30 cm H2O in
patients with ARDS. Thus, reduced tidal volumes are associated with the greatest improvement in
outcome after ARDS of any intervention subjected to a random-ized clinical
trial.
If
possible, the FIO2 should be maintained at 0.5 or less, primarily by
increasing PEEP above the inflection point (see Figure 57–6). Other maneuvers
to improve oxygenation include the use of inhaled nitric oxide, inhaled
prostacyclin or prostaglan-din E1 (PGE1), and ventilation
in the prone posi-tion. These three techniques improve oxygenation in many
patients with acute lung injury, but they are not risk free and they have not
been associated with an improvement in survival. A recent meta-analysis has
concluded that moderate doses of cor-ticosteroids likely improve morbidity and
mortality outcomes in ARDS, but the underlying data remain controversial.
Morbidity and mortality from ARDS usually arise
from the precipitating cause or from complica-tions rather than from the
respiratory failure itself. Among the most common serious complications are
sepsis, renal failure, and gastrointestinal hem-orrhage. Nosocomial pneumonia
is particularly common in patients with a protracted course and is often
difficult to diagnose; antibiotics are generally indicated when there is a high
index of suspicion (fever, purulent secretions, leukocytosis, and change in
chest radiograph). Protected specimen brushings and bronchoalveolar lavage sampling
via a flexible bronchoscope may be useful. Breach of mucocuta-neous barriers by
various catheters, malnutrition, and altered host immunity contribute to a
frequent incidence of infection. Kidney failure may result from various
combinations of volume depletion, sepsis, or nephrotoxins. Kidney failure
substantially increases the mortality rate for ARDS (to >60%).
Prophylaxis for gastrointestinal hemorrhage with
sucralfate, antacids, H2 blockers, or proton pump inhibitors is
recommended.
Related Topics