Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Critical Care
Discontinuing Mechanical Ventilation
Discontinuing
Mechanical Ventilation
There are two phases to discontinuing mechanical ventilation. In the
first, “readiness testing,” so-called weaning parameters and other subjective
and objec-tive assessments are used to determine whether the patient can
sustain progressive withdrawal of mechanical ventilator support. The second
phase, “weaning” or “liberation,” describes the way in which mechanical support
is removed.
Readiness testing should include determining
whether the process that necessitated mechanical ventilation has been reversed
or controlled. Com-plicating factors such as bronchospasm, heart fail-ure, infection,
malnutrition, metabolic acidosis or alkalosis, anemia, increased CO 2 production due to increased carbohydrate
loads, altered mental status, and sleep deprivation should be adequately
treated. Underlying lung disease and respiratory muscle wasting from prolonged
disuse often complicate weaning. Patients who fail to wean despite apparent
readiness often have COPD or chronic heart failure.
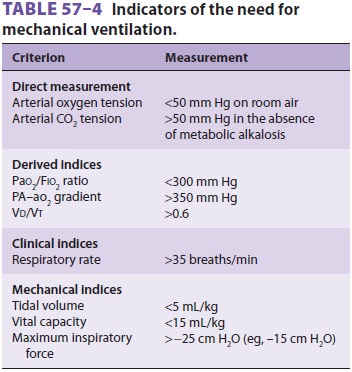
Weaning (or liberation) from mechanical
venti-lation should be considered when patients no longer meet general criteria
for mechanical ventilation (see Table 57–4). In general, this occurs when
patients have a pH greater than 7.25, show adequate arte-rial oxygen saturation
while receiving FIO2 less than 0.5, are able to spontaneously breathe, are hemo-dynamically
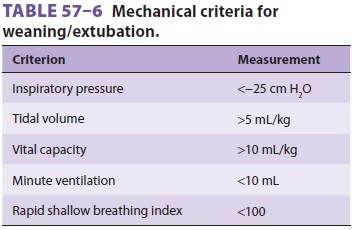
stable, and have no current signs of myocardial ischemia. Additional mechanical
indi-ces have also been suggested (Table 57–6).
Useful weaning parameters include arterial blood gas ten-sions, respiratory
rate, and rapid shallow breathing index (RSBI, see). Intact airway reflexes and
a cooperative patient are also mandatory prior to completion of the weaning and
extubation unless the patient will retain a cuffed tracheostomy tube.
Similarly, adequate oxygenation (arterial oxygen saturation >90% on 40–50% O2 with <5 cm H2O of PEEP) is imperative prior to extubation. When the patient is weaned
from mechanical ventilation and extubation is planned, the RSBI is frequently
used to help predict who can be successfully weaned from mechanical ventilation
and extubated. With the patient breathing spontaneously on a Τ-piece, the VT (in liters) and respiratory
rate (f) are measured:
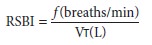
Patients with an RSBI less than 100 can be success-fully extubated.
Those with an RSBI greater than 120 should retain some degree of mechanical
ventilator support.
The common techniques to wean a patient from the ventilator include
SIMV, pressure sup-port, or periods of spontaneous breathing alone on a Τ-piece or on low levels of CPAP.
Mandatory minute ventilation has also been suggested as an ideal weaning
technique, but experience with it is limited. Finally, many institutions use
“automated tube compensation” to provide just enough pres-sure support to compensate
for the resistance of breathing through an endotracheal tube. Newer mechanical
ventilators have a setting that will auto-matically adjust gas flows to make
this adjustment. In practice in adults breathing through conven-tionally sized
tubes (7.5–8.5), the adjustment will typically amount to pressure support of 5
cm H2O and PEEP of 5 cm H2O.
Weaning with SIMV
With SIMV the number of mechanical breaths is progressively decreased
(by 1–2 breaths/min) as long as the arterial CO2 tension and respiratory rate
remain acceptable (generally <45–50 mm
Hg and <30 breaths/min, respectively).
If pressure sup-port is concomitantly used, it should generally be reduced to
5–8 cm H 2O. In patients with acid–base disturbances or chronic CO2
retention, arterial blood pH (>7.35) is
more useful than CO 2 tension. Blood gas
measurements can be checked after a minimum of 15–30 min at each setting. When
an IMV of 2–4 breaths is reached, mechanical ventila-tion is discontinued if
arterial oxygenation remains acceptable.
Weaning with PSV
Weaning with PSV alone is accomplished by
gradu-ally decreasing the pressure support level by 2–3 cm H2O while VT, arterial blood gas tensions, and
respi-ratory rate are monitored (using the same criteria as for IMV). The goal
is to try to ensure a VT of 4–6 mL/ kg and an f of less than 30 with acceptable PaO2 and PaCO2. When a pressure support level of 5–8 cm H2O is reached, the patient is considered weaned.
Weaning with a T-Piece or CPAP
Τ-piece trials allow observation while the
patient breathes spontaneously without any mechanical breaths. The Τ-piece
attaches directly to the tracheal tube or tracheostomy tube and has corrugated
tub-ing on the other two limbs. A humidified oxygen–air mixture flows into the
proximal limb and exits from the distal limb. Sufficient gas flow must be given
in the proximal limb to prevent the mist from being completely drawn back at
the distal limb during inspiration; this ensures that the patient is receiving
the desired oxygen concentration. The patient is observed closely during this
period; obvious new signs of fatigue, chest retractions, tachypnea,
tachy-cardia, arrhythmias, or hypertension or hypotension should terminate the
trial. If the patient appears to tolerate the trial period and the RSBI is less
than 100, mechanical ventilation can be discontinued perma-nently. If the
patient can also protect and clear the airway, the tracheal tube can be
removed.
If the patient has been intubated for a
pro-longed period or has severe underlying lung disease, sequential Τ-piece trials may be necessary. Periodic
trials of 10–30 min are initiated and progressively increased by 5–10 min or
longer per trial as long as the patient appears comfortable and maintains
acceptable arterial blood gas measurements.
Many patients develop progressive atelectasis during prolonged Τ-piece trials. This may reflect the
absence of a normal “physiological” PEEP when the larynx is bypassed by a
tracheal tube. If this is a concern, spontaneous breathing trials on low levels
(5 cm H2O) of CPAP can be tried. The CPAP helps maintain FRC and prevent
atelectasis.
Related Topics