Chapter: Essentials of Anatomy and Physiology: Respiratory System
Rhythmic Breathing
RHYTHMIC BREATHING
The normal rate of breathing in adults is between 12 and 20 breaths per minute. In children, the rates are higher and may vary from 20 to 40 per minute. The rate of breathing is determined by the number of times respiratory muscles are stimulated. The basic rhythm of breathing is controlled by neurons within the medulla oblongata that stimulate the muscles of respiration. An increased depth of breathing results from stronger contractions of the respiratory muscles caused by recruitment of muscle fibers and increased frequency of stimulation of muscle fibers.
Respiratory Areas in the Brainstem
Neurons involved with respiration are located in the brainstem. The neurons that are active during inspiration and those active during expiration are intermingled in these areas.
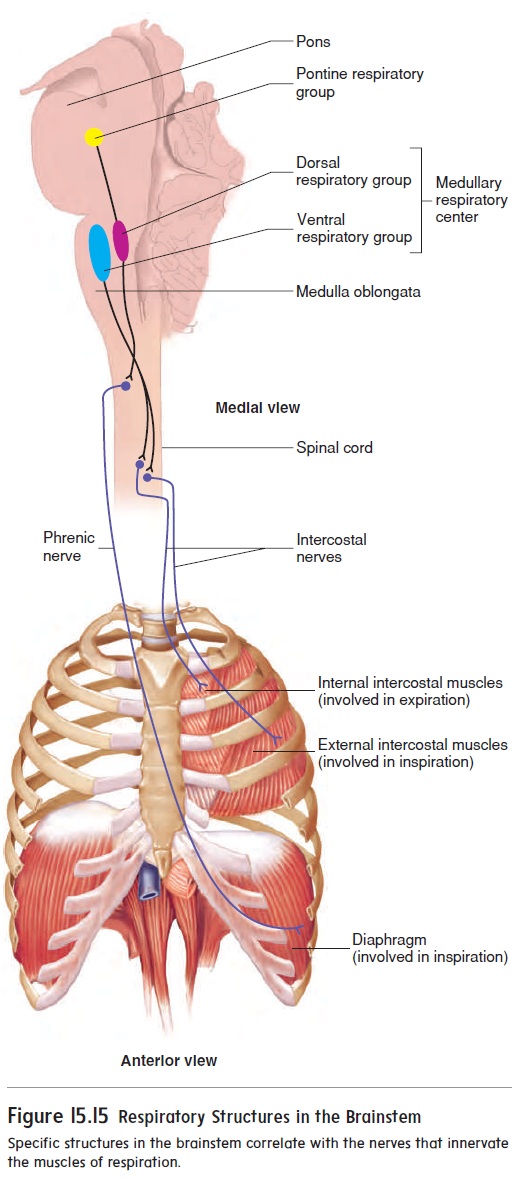
The medullary respiratory center consists of two dorsalrespiratory groups, each forming a longitudinal column of cellslocated bilaterally in the dorsal part of the medulla oblongata, and two ventral respiratory groups, each forming a longitudinal col-umn of cells located bilaterally in the ventral part of the medulla oblongata (figure 15.15). The dorsal respiratory group is primarily responsible for stimulating contraction of the diaphragm. The ven-tral respiratory group is primarily responsible for stimulating the external intercostal, internal intercostal, and abdominal muscles. A part of the ventral respiratory group, the pre-Bötzinger complex, is now known to establish the basic rhythm of breathing.
The pontine respiratory group is a collection of neurons in the pons (figure 15.15). It has connections with the medullary respiratory center and appears to play a role in switching between inspiration and expiration.
Generation of Rhythmic Breathing
The medullary respiratory center generates the basic pattern of spontaneous, rhythmic breathing. Although the precise mecha-nism is not well understood, the generation of rhythmic breathing involves the integration of stimuli that start and stop inspiration.
1. Starting inspiration. The neurons in the medullary respiratorycenter that promote inspiration are continuously active. The medullary respiratory center constantly receives stimulation from many sources, such as receptors that monitor blood gas levels and the movements of muscles and joints. In addition, stimulation can come from parts of the brain concerned with voluntary respiratory movements and emotions. When the inputs from all these sources reach a threshold level, somatic nervous system neurons stimulate respiratory muscles via action potentials, and inspiration starts.
2. Increasing inspiration. Once inspiration begins, more andmore neurons are activated. The result is progressively stronger stimulation of the respiratory muscles, which lasts for approximately 2 seconds (s).
3. Stopping inspiration. The neurons stimulating the musclesof respiration also stimulate the neurons in the medullary respiratory center that are responsible for stopping inspiration. The neurons responsible for stopping inspiration also receive input from the pontine respiratory neurons, stretch receptors in the lungs, and probably other sources. When the inputs to these neurons exceed a threshold level, they cause the neurons stimulating respiratory muscles to be inhibited. Relaxation of respiratory muscles results in expiration, which lasts approximately 3 s. The next inspiration begins with step 1.
Although the medullary neurons establish the basic rate and depth of breathing, their activities can be influenced by input from other parts of the brain and from peripherally located receptors.
Nervous Control Of Breathing
Higher brain centers can modify the activity of the respiratory center (figure 15.16a). For example, controlling air movements out of the lungs makes speech possible, and emotions can make us sob or gasp. In addition, breathing can be consciously controlled—that is, it is possible to breathe or to stop breathing voluntarily. Some people can hold their breath until they lose consciousness due tolack of O2 in the brain. Children have used this strategy to encour-age parents to give them what they want. However, as soon as conscious control of respiration is lost, automatic control resumes, and the person starts to breathe again.
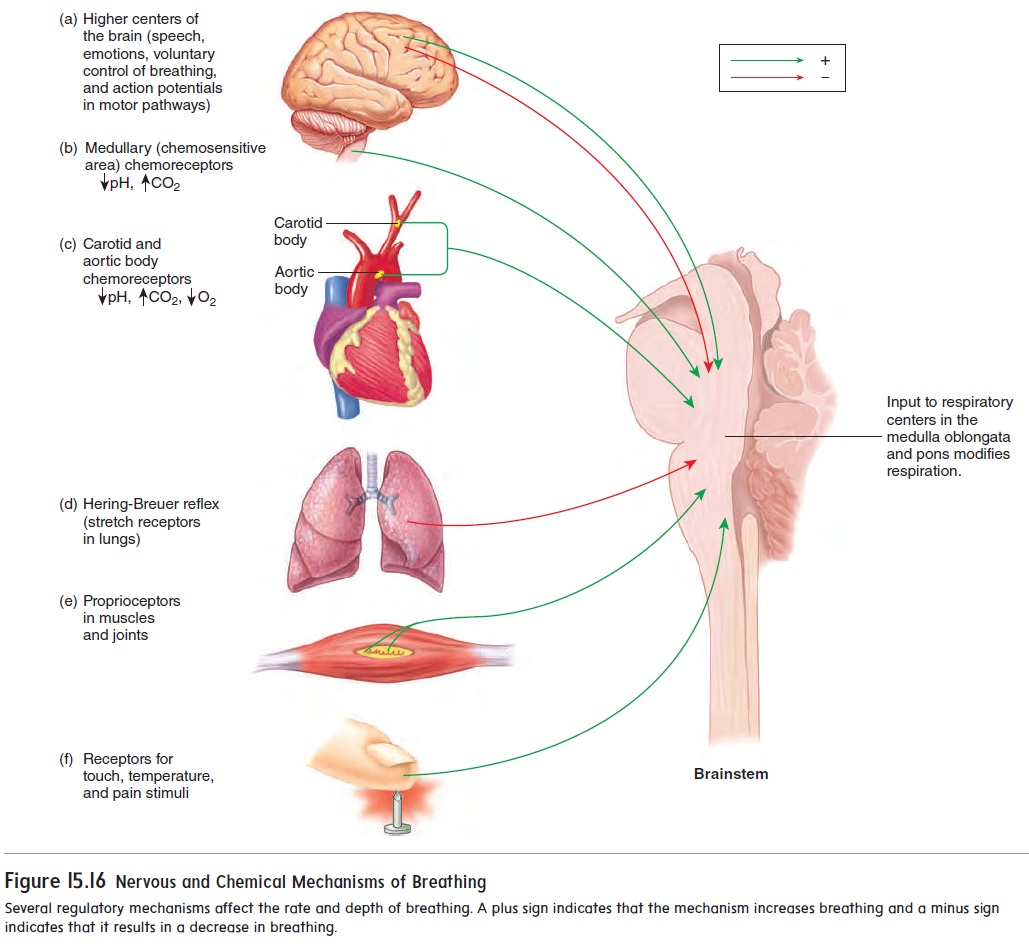
Several reflexes, such as sneeze and cough reflexes, can mod-ify breathing. The Hering-Breuer (her′ ing broy′ er) reflex supports rhythmic respiratory movements by limiting the extent of inspiration (figure 15.16d). As the muscles of inspiration contract, the lungs fill with air. Sensory receptors that respond to stretch are located in the lungs, and as the lungs fill with air, the stretch receptors are stimu-lated. Action potentials from the lung stretch receptors are then sent to the medulla oblongata, where they inhibit the respiratory center neurons and cause expiration. In infants, the Hering-Breuer reflex plays an important role in regulating the basic rhythm of breathing and in preventing overinflation of the lungs. In adults, however, the reflex is important only when the tidal volume is large, as occurs during heavy exercise.
Touch, thermal, and pain receptors in the skin also stimulate the respiratory center, which explains why we gasp in response to being splashed with cold water or being pinched (figure 15.16e,f ).
Chemical Control of Breathing
During cellular respiration, the body’s cells consume O2 and pro-duce CO2 . The primary function of the respiratory system is to add O2 to the blood and to remove CO2 from the blood.
Surprisingly, the level of CO2, not O2, in the blood is the major driving force regulating breathing. Even a small increase in the CO2 level (hypercapnia), such as when holding your breath, results in a powerful urge to breathe. The mechanism by which CO2 in the blood stimulates breathing involves the change in pH that accompa-nies an increase in CO2 levels. Receptors in the medulla oblongata calledchemoreceptors are sensitive to small changes in H+ con-centration. Recall from the section “Carbon Dioxide Transport and Blood pH” that blood CO2 combines with water, which increases H+concentration. Thus, it is the H+ that is detected by the medul-lary chemoreceptors (figure 15.16b).
Although O2 levels are not the major driving force of breath-ing, there are O2-sensitive chemoreceptors in the carotid and aortic bodies (figure 15.16c). When blood O2 levels decline to a low level (hypoxia) such as during exposure to high altitude, emphysema, shock, and asphyxiation, the aortic and carotid bodies are strongly stimulated. They send action potentials to the respiratory center and produce an increase in the rate and depth of breathing, which increases O2 diffusion from the alveoli into the blood.
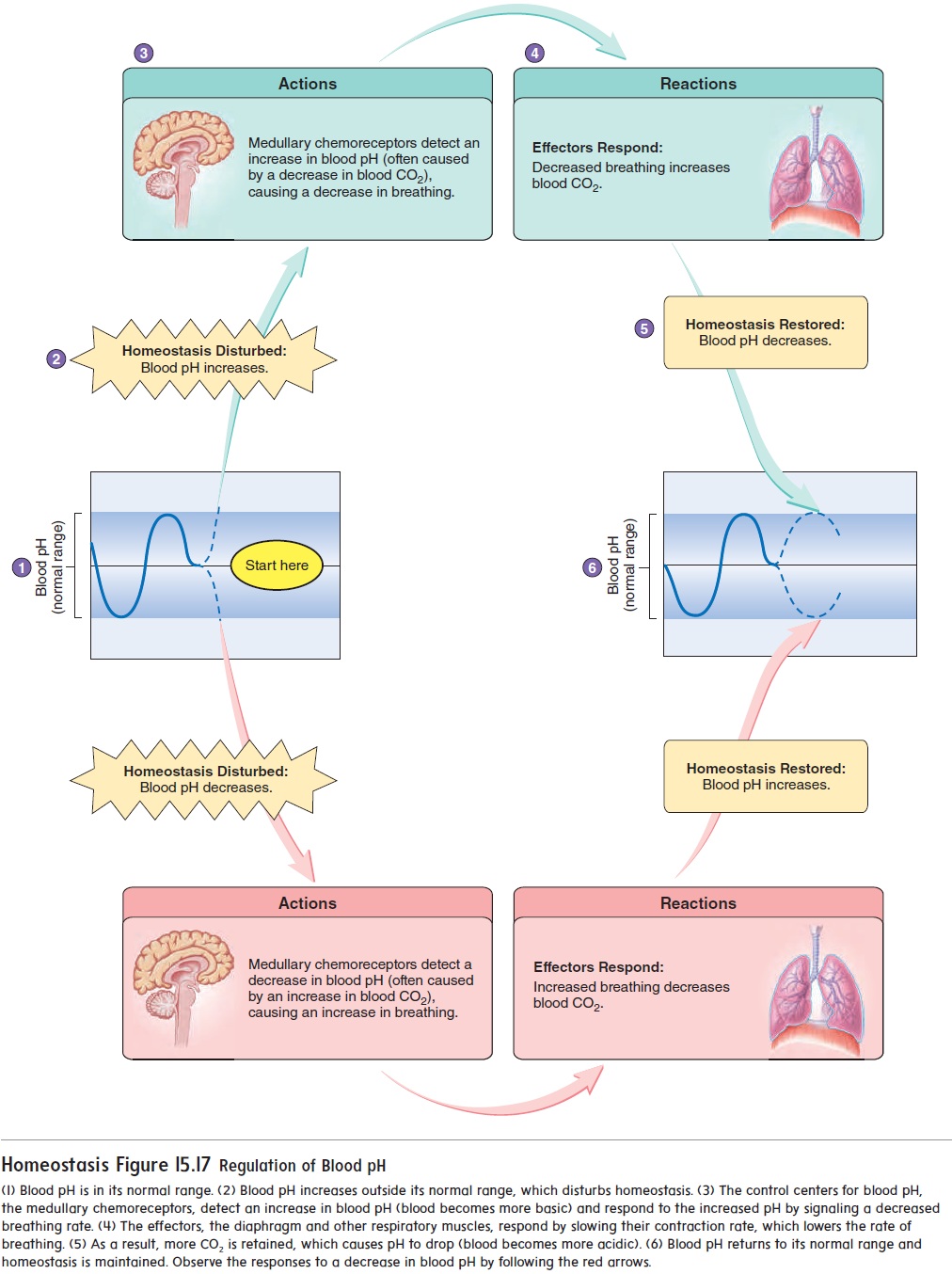
Because CO2 levels affect blood pH, the medullary chemore-ceptors are important for more than just regulating breathing rate; the medullary chemoreceptors play a crucial role in maintaining blood pH. Figure 15.17 depicts the role breathing rate has on blood pH. If blood CO2 levels decrease, such as during more rapid breathing, blood pH will increase (become more basic). Thus, the homeostatic mechanism is that the medullary chemoreceptors signal a decreased breathing rate, which retains CO2 in the blood. More CO2 in the blood causes H+ levels to increase, which causes blood pH to decrease to normal levels. Alternatively, if blood CO2 levels increase, such as during increased physical activity when the body’s cells are producing more CO2 as waste, blood pH will decrease (become more acidic). The medullary chemoreceptors will detect the elevated H+ and signal a faster breathing rate. As breathing rate goes up, more CO2 will diffuse out of the blood and blood pH will return to normal. Thus, CO2 levels are very influ-ential on breathing rate. The opposite is also true, which is why hyperventilation without accompanying increases in CO2 levels due to physical exercise can cause someone to pass out.
Effect Of Exercise On Breathing
The mechanisms by which breathing is regulated during exercise are controversial, and no single factor can account for all the observed responses. Breathing during exercise can be divided into two phases:
1. Breathing increases abruptly. At the onset of exercise,the rate of breathing immediately increases. This initial increase can be as much as 50% of the total increase that will occur.
The immediate increase occurs too quickly to be explained by changes in metabolism or blood gases. As axons pass from the motor cortex of the cerebrum through the motor pathways, numerous collateral fibers project to the respiratory center. During exercise, action potentials in the motor pathways stimulate skeletal muscle contractions, and action potentials in the collateral fibers stimulate the respiratory center (see figure 15.16).
Furthermore, during exercise, body movements stimulate proprioceptors in the joints of the limbs. Nerve fibers from these proprioceptors extend to the spinal cord to connect with sensory nerve tracts ascending to the brain. Collateral fibers from these nerve tracts connect to the respiratory center; therefore, movement of the limbs has a strong stimulatory influence on the respiratory center (see figure 15.16e).
There may also be a learned component in the breathing response during exercise. After a period of training, the brain“learns” to match breathing with the intensity of the exercise. Well-trained athletes match their respiratory movements more efficiently with their level of physical activity than do untrained individuals. Thus, centers in the brain involved in learning have an indirect influence on the respiratory center, but the exact mechanism is unclear.
2. Breathing increases gradually. After the immediate increasein breathing, breathing continues to increase gradually and then levels off within 4–6 minutes after the onset of exercise. Factors responsible for the immediate increase in breathing may play a role in the gradual increase as well.
Despite large changes in O2 consumption and CO2 produc-tion during exercise, the average arterial O2, CO2, and pH levels remain constant and close to resting levels as long as the exercise is aerobic . This suggests that changes in blood gases and pH do not play an important role in regulating breathing during aerobic exercise. However, during exercise, the values of arterial O2, CO2, and pH levels rise and fall more than they do at rest.
Thus, even though their average values do not change, their oscillations may be a signal for helping control breathing.
The highest level of exercise that can be performed without causing a significant change in blood pH is the anaerobic thresh-old. If the exercise intensity becomes high enough to exceed theanaerobic threshold, skeletal muscles produce lactate through theanaerobic process of anaerobic respiration (see figure 17.5). Lactate released into the blood contributes to a decrease in blood pH, which stimulates the carotid bodies, resulting in increased breathing. In fact, ventilation can increase so much that arterial CO2 levels fall below resting levels, and arterial O2 levels rise above resting levels.
Related Topics