Chapter: Essentials of Anatomy and Physiology: Respiratory System
Respiratory Volumes and Capacities
Respiratory Volumes and Capacities
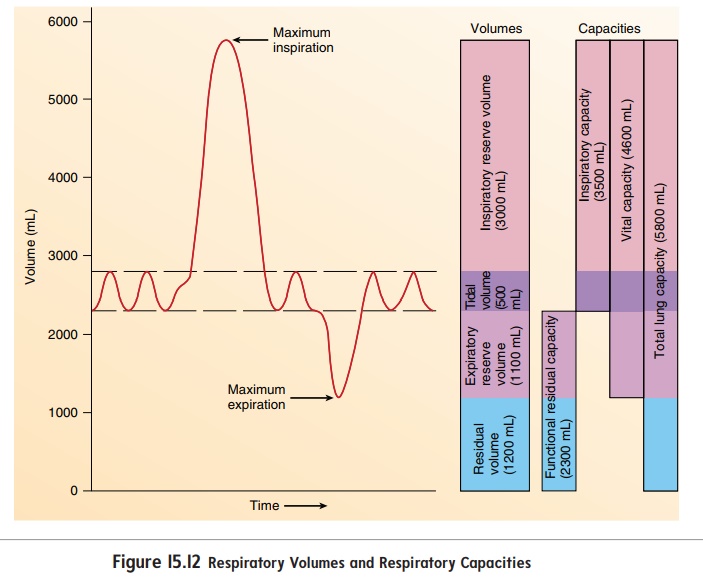
Spirometry (sp -rom′-tr ) is the process of measuring volumes of air that move into and out of the respiratory system, and thespirometer (sp -rom′-ter) is the device that measures these respiratory volumes. Measurements of the respiratory volumes can provide information about the health of the lungs. Respiratoryvolumes are measures of the amount of air movement during dif-ferent portions of ventilation, whereas respiratory capacities are sums of two or more respiratory volumes. The four respiratory volumes and their normal values for a young adult male are shown in figure 15.12:
1. Tidal volume is the volume of air inspired or expired witheach breath. At rest, quiet breathing results in a tidal volume of about 500 milliliters (mL).
2. Inspiratory reserve volume is the amount of air that canbe inspired forcefully beyond the resting tidal volume (about 3000 mL).
3. Expiratory reserve volume is the amount of air that canbe expired forcefully beyond the resting tidal volume (about 1100 mL).
4. Residual volume is the volume of air still remaining in therespiratory passages and lungs after maximum expiration (about 1200 mL).
The tidal volume increases when a person is more active. Because the maximum volume of the respiratory system does not change from moment to moment, an increase in the tidal volume causes a decrease in the inspiratory and expiratory reserve volumes.
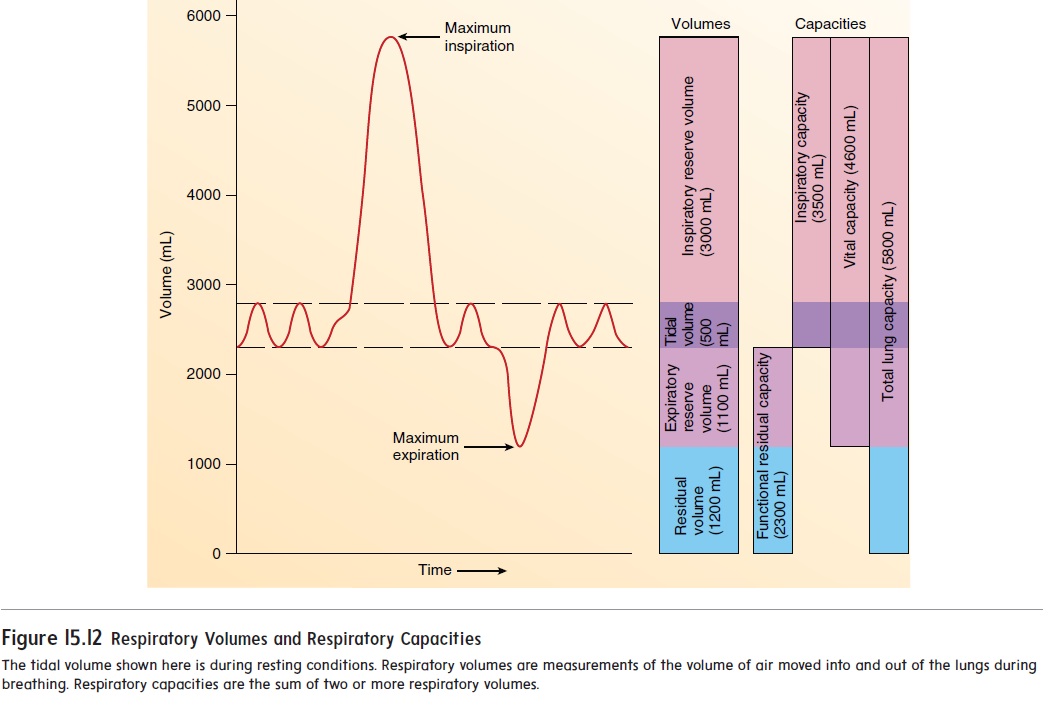
Values of respiratory capacities, the sum of two or more pul-monary volumes, are shown in figure 15.12:
1. Functional residual capacity is the expiratory reservevolume plus the residual volume. This is the amount of air remaining in the lungs at the end of a normal expiration (about 2300 mL at rest).
2. Inspiratory capacity is the tidal volume plus the inspiratoryreserve volume. This is the amount of air a person can inspire maximally after a normal expiration (about3500 mL at rest).
3. Vital capacity is the sum of the inspiratory reserve volume,the tidal volume, and the expiratory reserve volume. It is the maximum volume of air that a person can expelfrom the respiratory tract after a maximum inspiration (about 4600 mL).
4. Total lung capacity is the sum of the inspiratory andexpiratory reserves and the tidal and residual volumes (about 5800 mL). The total lung capacity is also equal to the vital capacity plus the residual volume.
Factors such as sex, age, and body size influence the respira-tory volumes and capacities. For example, the vital capacity of adult females is usually 20–25% less than that of adult males. The vital capacity reaches its maximum amount in young adults and gradually decreases in the elderly. Tall people usually have a greater vital capacity than short people, and thin people have a greater vital capacity than obese people. Well-trained athletes can have a vital capacity 30–40% above that of untrained people. In patients whose respiratory muscles are paralyzed by spinal cord injury or diseases such as poliomyelitis or muscular dystrophy, the vital capacity can be reduced to values not consistent with survival (less than 500–1000 mL).
The forced expiratory vital capacity is the rate at which lung volume changes during direct measurement of the vital capacity. It is a simple and clinically important pulmonary test. The individual inspires maximally and then exhales maximally as rapidly as possible into a spirometer. The spirometer records the volume of air expired per second. This test can help identify conditions in which the vital capacity might not be affected but the expiratory flow rate is reduced. Abnormalities that increase the resistance to airflow slow the rate at which air can be forced out of the lungs. For example, in people who have asthma, contraction of the smooth muscle in the bronchioles increases the resistance to airflow. In people who have emphysema, changes in the lung tissue result in the destruction of the alveolar walls, Âcollapse of the bron-chioles, and decreased elasticity of the lung tissue. The collapsed bronchioles increase the resistance to airflow. In people who have chronic bronchitis, the air passages are inflamed. The swelling, increased mucus secretion, and gradual loss of cilia result in narrowed bronchioles and increased resistance to airflow.
Related Topics