Chapter: Medicine and surgery: Genitourinary system
Renal tubular syndromes - Tubular and interstitial diseases
Renal tubular syndromes
Definition
These are syndromes in which a metabolic disorder of tubular function is the main feature. They may be inherited or acquired.
Aetiology
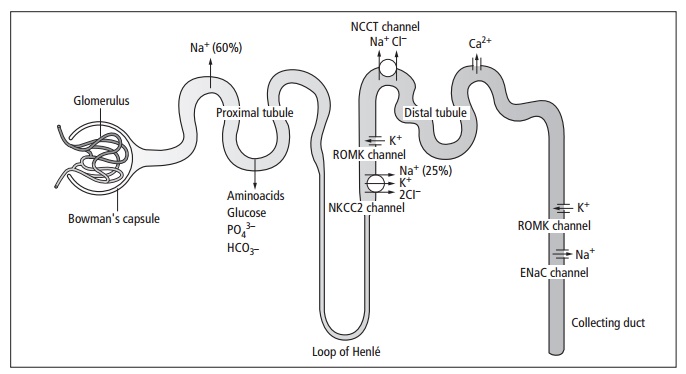
They may be classified as single or multiple defects, or they can be grouped according to the part of the nephron affected (see Fig. 6.9). See also Renal Tubular Acidosis (see below). The single defects are discussed here.
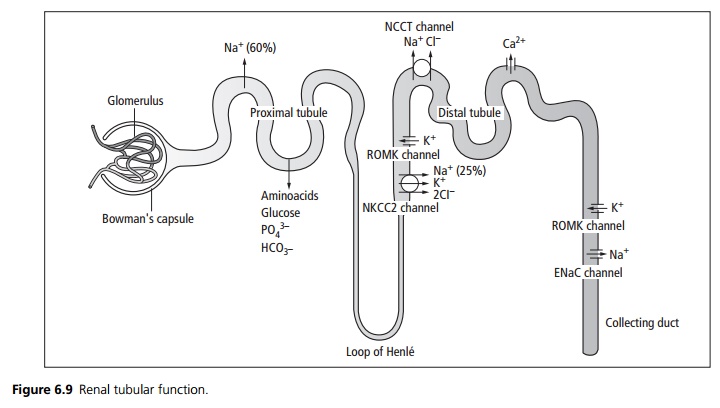
Proximal tubule: The proximal tubule is the site of maximal reabsorption of glucose and sodium. Water and anions such as aminoacids follow sodium. Osmotic diuretics and carbonic anhydrase inhibitors act at this site. Disorders of the proximal tubule may lead to one or more of the following syndromes:
· Renal glycosuria is an autosomal recessive inherited condition characterised by glycosuria with normal blood glucose. There is impaired reabsorption of glucose in the proximal tubules, with no clinical sequelae. Glycosuria is a normal response during pregnancy.
· Aminoaciduria may affect only one amino acid or several. The most important single defect is cystinuria, an autosomal recessive condition which predisposes to urinary stone formation. Treatment is with high fluid intake and alkali ingestion, because the cystine is more soluble in alkaline conditions. Drugs such as penicillamine may be used to form complexes with the cystine. In Fanconi syndrome (which may be an inherited juvenile form or acquired in adults) there is defective reabsorption of most aminoacids, glucose, phosphate and bicarbonate. There may be potassium depletion, polyuria and immunodeficiency secondary to immunoglobulin loss. Phosphate loss leads to vitamin D resistant rickets in childhood, and osteomalacia in adults.
· Phosphate transport defects: There are several types, usually X-linked, although occasional sporadic inherited or acquired cases do occur. They cause inappropriate loss of phosphate from the tubules and result in hypophosphataemia and vitamin D resistant rickets (VDDR). Treatment is with oral phosphate supplements with vitamin D or 1,25 dihydroxyvitamin D
· (calcitriol).
Thick ascending loop of Henle: Sodium is pumped out of the lumen in the ascending loop, water is drawn out of the descending loop by osmosis. This creates a concentration gradient within the medulla of the kidney, which draws water out of the collecting duct and hence concentrates the urine. Loop diuretics such as furosemide act from within the lumen of the ascending loop binding to the chloride site of the NKCC2 channel. This interferes with the pump reducing the concentration gradient resulting in more dilute urine.
· Bartter type I syndrome is an autosomal recessive defect in the gene encoding the NKCC2 pump. It results in high urinary sodium loss, dehydration, secondary hyperaldosteronism and hypokalaemic alkalosis. There is hypercalciuria and nephrocalcinosis.
· Bartter type II syndrome is an autosomal recessive defect in the gene encoding the ROMK channel. Decreased potassium excretion causes hyperkalaemia, which interferes with the action of the NKCC2 pump. This results in a similar syndrome of sodium loss, dehydration and hypercalciuria as Bartter type I; how-ever, hypokalaemia only occurs after treatment with sodium supplements.
Distal convoluted tubule: Thiazide diuretics act from within the lumen of the distal tubule binding to the chloride site of the NCCT channel reducing sodium and water reabsorption. Calcium reabsorption is increased leading to hypercalcaemia.
· Gittleman syndrome is an autosomal recessive mutation in the gene encoding the NCCT channel. As there is increased sodium in the urine reaching the collecting duct there is exchange of sodium for potassium in the collecting duct resulting in a hypokalaemic metabolic alkalosis.
Collecting duct: At the collecting duct there is reabsorption of sodium in exchange for potassium excretion. This is under the influence of aldosterone which increases sodium (and hence water) reabsorption. Spironolactone and amiloride affect this exchange and hence increase urinary water and sodium loss. In contrast to other diuretics, these cause potassium reabsorption and are termed potassiumsparing diuretics. The permeability of the collecting duct is under the influence of anti diuretic hormone (ADH or vasopressin).
· In diabetes insipidus (see also page 445) the action of ADH is impaired. This results in excessive water loss in the urine.
Related Topics