Chapter: Medicine and surgery: Genitourinary system
Nephrotic syndrome - Glomerular disease
Nephrotic syndrome
Definition
Nephrotic syndrome is defined as proteinuria (>3 g/24 hour), hypoalbuminaemia and oedema. See also proteinuria.
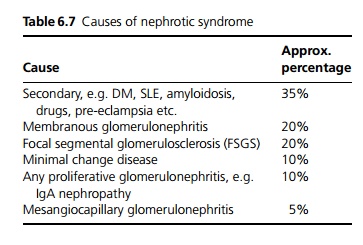
Aetiology
The most common causes of nephrotic syndrome in adults (apart from secondary causes) are membranous nephropathy and focal segmental glomerulosclerosis (see Table 6.7). In children, minimal change disease is more common, accounting for up to 90% of cases under the age of 10 years.
Drugs that can cause nephrotic syndrome include NSAIDs, gold and other heavy metals, and penicillamine.
Pathophysiology
The glomerular basement membrane (GBM) becomes more permeable than usual so protein leaks out into the urine. There is no acute inflammatory response either because there are no immune deposits (such as in minimal change nephropathy, focal segmental glomerulosclerosis and in amyloidosis) or the immune complexes are subepithelial (such as in membranous nephropathy).
Haematuria and renal failure are therefore usually minor or absent.Albumin is the main protein lost, but clotting factors, transferrin and other proteins may be lost as well. The liver is able to synthesise enough albumin to compensate for the losses initially, but if protein losses are large, hypoalbuminaemia results. Peripheral oedema is the result of a fall in plasma oncotic pressure, so that fluid stays in the tissues, and also sodium retention by the kidney.
Clinical features
Gradual development of swelling of eyelids, peripheral oedema, ascites and pleural effusions. The urine may be frothy due to proteinuria. There may be relevant history of drugs, other past medical history or a family history of renal disease.
Complications
Venous thrombosis and pulmonary embolism due to loss of antithrombin III in the urine, lowered plasma volume and increased clotting factors (II, V, VII, VIII and X).
Renal vein thrombosis may occur particularly in patients with a very low serum albumin (<20 g/L) or membranous nephropathy. This is usually asymptomatic, the first sign may be a pulmonary embolus, or it may present acutely due to venous infarction with flank pain, haematuria and renal impairment.
Infection, particularly streptococcal infections, possibly due to low levels of IgG.
Hypercholesterolaemia is thought to occur due to increased hepatic lipoprotein synthesis as a response to decreased plasma oncotic pressure. Reduced metabolism also plays a part in hypercholesterolaemia and hypertriglyceridaemia.
Acute renal failure may occur due to hypovolaemia (often diureticinduced), or in some cases there is both glomerular and tubular damage. Most causes of nephrotic syndrome do not cause ARF.
Loss of specific binding proteins, e.g. transferrin, leading to ironresistant hypochromic anaemia.
Protein malnutrition.
Investigations
Measured or calculated creatinine clearance and total protein.
Urine microscopy.
Bence Jones protein (to look for myeloma).
Blood for U&Es, albumin, cholesterol, FBC, ESR, CRP. A variety of other blood tests may be able to suggest
a diagnosis, such as serum protein electrophoresis, ANA, anti-dsDNA, C3, C4.
Renal biopsy is indicated in most cases, but children and teenagers without haematuria, hypertension or renal impairment are very likely to have minimal change disease, so if a trial of steroids leads to full remission, biopsy may be avoided.
Management
Treatment of the underlying cause.
· ACE-inhibitors are used to lower intraglomerular pressure. This reduces the proteinuria and slows progression of renal disease.
· Sodium restriction and diuretics are used to relieve oedema, but with care to avoid precipitating prerenal failure, due to intravascular hypovolaemia.
· Dietary protein must be sufficient to compensate for urinary losses.
· Treat complications: Hyperlipidaemia responds to treatment of the nephrotic syndrome, although HMG CoA reductase inhibitors (statins) are often needed. Consider anticoagulation and prophylactic penicillin.
Related Topics