Chapter: Medicine and surgery: Genitourinary system
Acute renal failure - Disorders of the kidney
Acute renal failure
Definition
A deterioration of renal function (loss of GFR) over a period of days to weeks.
Aetiology/pathophysiology
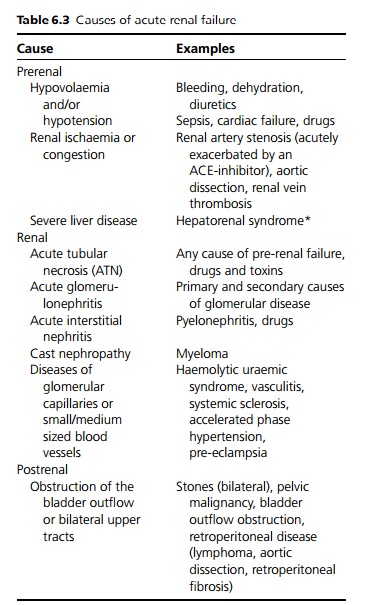
The causes may be divided into prerenal, renal and postrenal, whilst they all have different mechanisms, the result is loss of the three functions of the kidney: fluid and electrolyte balance, excretion of waste products and toxins, and hormone synthesis (see Table 6.3).
Clinical features
The main clinical features are usually those of the under-lying cause together with symptoms and signs caused by the renal failure. Acute renal failure (ARF) may be difficult to differentiate from chronic renal failure (CRF) without a recent onset in symptoms of an underlying cause, e.g. loin pain, a previous serum creatinine measurement or further investigations.
· In asymptomatic patients, ARF may be detected by a rise in plasma creatinine or abnormality on urine dipstick.
· Reduced urine output or a change in urine appearance. Complete anuria is only seen with bladder out-flow obstruction, bilateral (or unilateral in a single functioning kidney) ureteric obstruction.
· Loin pain – this is suggestive of a renal stone (or other cause of obstruction), pyelonephritis or renal infarction.
· Anorexia, vomiting, fever, malaise, hiccoughs, confusion, seizures.
· Hyperventilation may be due to hypoxia or respiratory compensation for metabolic acidosis.
It is important to assess the volume status by assessing blood pressure, jugular venous pressure, skin turgor, ankle or sacral oedema and pulmonary oedema. Hyper-tension may be a feature.
Complications
Hyperkalaemia may cause cardiac arrhythmias and sudden death. Fluid overload may cause cardiac failure, pulmonary oedema. Gastric erosions and GI bleeding are quite common. Uraemic pericarditis can rarely lead to tamponade. During recovery of ATN, there may be polyuria in which it is often difficult to maintain sufficient water and electrolyte input.
Investigations
The aims are to try to distinguish acute and chronic renal failure, between prerenal, renal or postrenal causes, as well as the underlying cause.
· Urgent urinalysis, followed by microscopy (to look for cells and casts) and culture.
· Urine sodium concentration. In prerenal failure, or in renal failure without tubular dysfunction the kidney will reabsorb sodium so that urinary sodium is less than 20 mmol/L (exceptions to this are in the presence of diuretics, in preexisting chronic renal failure). If there is tubular damage, then the ability of the kidney to concentrate sodium falls, so that urinary sodium rises to >40 mmol/L.
· Bloods
1. Anaemia (normochromic, normocytic if underly-ing disease or in chronic renal failure).
2. Raised urea, creatinine, K+ , urate.
3. Reduced Ca2+ with increased PO4.
4. Na+ may be high, normal or low.
5. Arterial/venous blood gas shows a metabolic acidosis usually with increased anion gap.
6. LFTs.
7. Creatine kinase (CK) – raised in myocardial infarction but also very high in rhabdomyolysis (muscle breakdown).
· ECG, chest X-ray.
· Renal imaging to exclude obstruction – a renal ultra-sound should be obtained as soon as possible to look for hydronephrosis (dilated renal pelvis, calyces and ureters) and for renal size.
· Consider further tests for causes of ARF if diagnosis still unclear. These include autoantibody profile, complement levels, blood and urine tests for myeloma and possibly a renal biopsy.
Management
Acute renal failure is an emergency, with possible life-threatening complications.
Reversible causes should be treated as soon as possible; withdraw any potentially nephrotoxic drugs, treat sepsis, malignant hypertension, and relieve any obstruction.
Fluid management
If volume depletion is causing renal failure then appropriate fluid replacement (usually colloid, crystalloid or blood) should be given. Fluid challenges may be required with regular review to ensure that the patient does not become fluid overloaded. Central venous pressure measurement may be helpful, but should not be relied upon over clinical assessment especially in the presence of cardiac or pulmonary disease. Urinary catheterisation is not always required, and carries a risk of introducing infection. Urine output should increase in response to filling. If it does not, and the patient is well filled, then there is likely to be concomitant renal ARF. If blood pressure remains low despite filling (such as due to cardiac insufficiency, sepsis), then additional treatment, usually inotropic support is needed with specialist help.
Once the patient is normovolaemic intravenous fluids should be reduced to maintenance levels to avoid precipitating fluid overload.
In fluid overload, or in oliguric renal failure high doses of furosemide may be effective in causing a diuresis. However, there is no good evidence that furosemide speeds the recovery from renal failure, and it should be avoided in those thought to have pre-renal failure.
Pulmonary oedema which does not respond to diuretics may have to be treated initially with vasodilators (intravenous GTN, diamorphine) and ventilatory support including non-invasive ventila-tion, but the only definitive treatment is haemodialysis or haemofiltration.
Hyperkalaemia
Treat severe hyperkalaemia (K > 6.0 mmol/L) urgently to avoid cardiac arrhythmias.
Stop any drugs that cause high potassium (ACE-inhibitors, spironalactone).
General measures
A multidisciplinary approach is required, involving physiotherapists, nurses and nutritionists.
Monitor fluid in/out, daily weight (this is a useful, accurate way of monitoring fluid balance).
Low salt and potassium diet. Ensure adequate nutrition.
Review all medication for dosages in renal failure.
Consider prophylaxis against gastrointestinal bleeding.
Referral to a renal physician should be considered if there are red cell casts or heavy proteinuria, if the diagnosis is unclear or if there is acute-on-chronic renal failure.
Indications for urgent dialysis
Persistent hyperkalaemia >6 mmol/L despite medical therapy
Severe acidosis
Refractory pulmonary oedema
Pericarditis, cardiac tamponade, encephalopathy (flap)
Rapidly progressive renal failure
Prognosis
Depends on underlying cause and concomitant medical conditions. Oliguric ARF has a higher mortality.
Related Topics