Chapter: Basic Radiology : Radiology of the Chest
Radiology of the Chest: Technique Selection
TECHNIQUE
SELECTION
The number of diseases and
clinical situations for which a chest radiograph may be indicated is so large
that an ex-haustive listing of individual indications is prohibitive. As a
general rule, however, conventional radiographs should be obtained for any
patient with symptoms suggesting dis-ease of the heart, lungs, mediastinum, or
chest wall. In ad-dition, a chest radiograph is indicated for patients with
systemic diseases that have a high likelihood of secondary involvement of those
structures. Examples of the former are pneumonia and congestive heart failure
and of the lat-ter are a primary extrathoracic neoplasm and connective tissue
disease.
In an acutely ill patient, the
portable chest radiograph is an invaluable tool for monitoring the patient’s
car-diopulmonary status. These radiographs are also used for monitoring of
life-support hardware, such as central venous access catheters, nasogastric tubes,
and endotra-cheal tubes.
Fluoroscopy provides real-time
imaging of the chest. Flu-oroscopy may be used to evaluate the motion of the
di-aphragm in a patient with suspected diaphragmatic paralysis. A paralyzed
hemidiaphragm has sluggish motion as the pa-tient breathes, and as the patient
takes in a quick breath of air, it moves paradoxically upward as the normal
hemidi-aphragm moves downward (“sniff test”). Fluoroscopy and fluoroscopically
positioned spot images are also useful for identification of calcification
within a pulmonary nodule, within coronary arteries, or within cardiac valves.
Fluoro-scopic guidance can also be used for percutaneous transtho-racic needle
biopsy of lung masses.
Because the three dimensions of
the thorax are captured on a single two-dimensional chest radiograph,
superimposi-tion of structures within the thorax may result in confusing
shadows. Because CT provides images without this overlap, it is frequently used
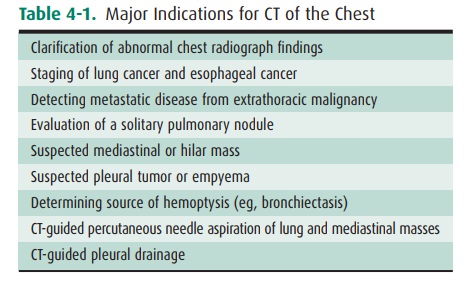
to clarify confusing shadows identified on conventional radiographs (Table
4-1). These examina-tions are also used to detect disease that is occult
because of small size or a hidden position. Because of its wider range of
density discrimination, CT can demonstrate mediastinal and chest wall
abnormalities earlier than is possible with conventional chest radiography.
Abnormalities of hilar structures can be identified on CT scans because of the
de-creased overlap of the complex structures of the hilum. CT scans of the
chest are routinely ordered for oncology pa tients, both for evaluation of the
extent of disease at presen-tation and for monitoring response to therapy or
progres-sion of disease. CT is useful for evaluation of the lungparenchyma, as
thin sections (1 to 2 mm thick) reveal great anatomic detail. Thin-section CT
(or high-resolution CT [HRCT]) may enable detection of occult pulmonary
parenchymal disease and may be used for following the course of known pulmonary
disease (Table 4-2). HRCT is especially useful in the diagnosis of interstitial
lung diseases. Additionally, CT angiography (CTA) of the chest is particu-larly
useful for the evaluation of vascular pathology as well as pulmonary embolus
(Table 4-3). Because intravenous contrast material can be administered,
vascular structures may be evaluated and the technique may be useful in
pa-tients with aortic dissection, aortic aneurysm, and superior vena caval
obstruction. Because the cost of CT is approxi-mately 10 to 20 times that of a PA
and lateral chest radi-ograph, CT is not practical for monitoring the course of
diseases on a daily basis.
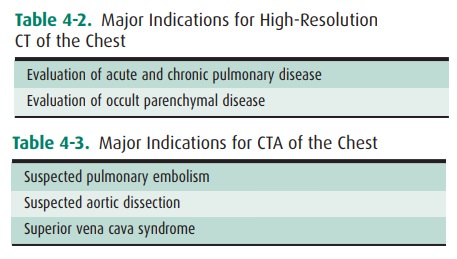
The diseases and situations for
which nuclear medicine techniques are helpful are determined for the most part
by the radioactive tracer, and these have been outlined in the technique
section (Table 4-4).
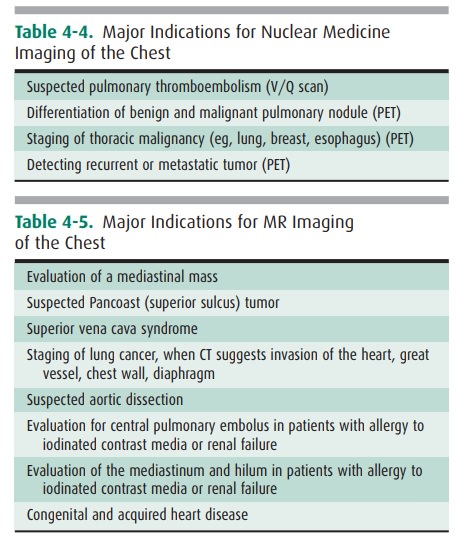
MR imaging of the thorax is most
commonly used for car-diovascular imaging, but there are indications for MR
imag-ing in mediastinal and pulmonary parenchymal imaging as well (Table 4-5).
MR is helpful when bronchogenic carcinoma is suspected of invading vascular
structures, including the cardiac chambers, pulmonary arteries and veins, and
the superior vena cava. In a patient with suspected Pancoast’s (superior
sulcus) tumor (Figure 4-9), MR imaging is pre-ferred to CT because of the
ability to obtain images in coronal and sagittal planes. The apex of the lung
can be difficult to evaluate on axial images alone because of partial-volume
effects.
Ultrasonography is useful for
imaging the soft tissues of the chest wall, heart, and pericardium, as well as
fluid collec-tions within the pleural space. Large, mobile pleural effusions
are usually aspirated without sonographic guidance, because these collect
predictably within dependent areas of the tho-rax. On the other hand, loculated
pleural fluid collections may be difficult to aspirate without guidance, and
the most appropriate entrance site may be marked with sonography for easier
access. Ultrasonography has been used for guidance for biopsy of peripheral
lung lesions as well.
Related Topics