Chapter: Basic Radiology : Radiology of the Chest
Exercise: Pulmonary Vascular Disease
EXERCISE 4-14.
PULMONARY VASCULAR DISEASE
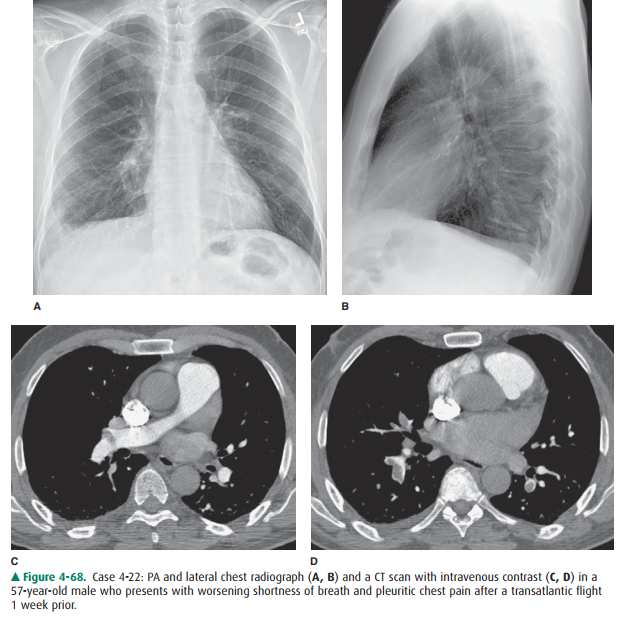
4-22. The most likely
cause for this patient’s dyspnea and pleuritic chest pain (Figure 4-68 A–D) is
A.
multifocal pneumonia.
B.
malignant pleural effusion.
C.
pulmonary embolism.
D.
septic emboli.
E.
drug-related pneumonitis.
Radiologic Findings
4-22. The chest x-ray
shows a wedge-shaped opacity in the periphery of the right lung base. There is
blunting of the right lateral costophrenic angle on the PA view of the chest.
The opacity could represent a Hampton’s hump in the clinical setting of
pulmonary embolus. Alternatively, pneumonia could have a similar presen-tation.
The CT scan demonstrates filling defects within the pulmonary arteries
bilaterally. At the levels shown, thromboemboli are visible within the right
main pul-monary artery extending into the right upper lobe pul-monary artery
(Figure 4-68 C) and within the basilar segmental arteries bilaterally (Figure
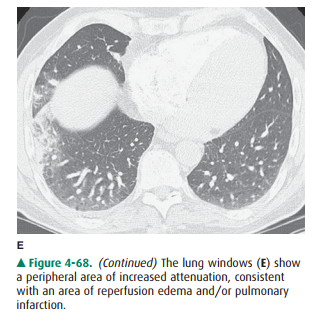
4-68 D). (C is the correct answer to Question 4-22.) The lung windows (Figure
4-68 E) show a peripheral area of increased at-tenuation, consistent with an
area of reperfusion edema and/or pulmonary infarction.
Discussion
Pulmonary thromboembolism can
occur as a result of deep venous thrombosis, typically from the veins of the
pelvis and lower extremities. These thrombi dislodge (em-bolize) and travel via
the inferior vena cava and right heart chambers to become trapped in the
tapering branches of the pulmonary arterial system. Because pulmonary em-bolism
often occurs without pulmonary infarction, the ap-pearance of the chest
radiograph is usually normal. The areas of lung deprived of pulmonary arterial
flow are per-fused by bronchial arterial collateral vessels. The chest
ra-diograph may demonstrate subtle signs of volume loss or a small pleural
effusion. Pulmonary opacities develop be-cause of microatelectasis within the
region of lung that has had an embolus, from edema as the blood flow is
restored via the bronchial circulation, or from hemorrhage within a pulmonary
infarction. Pulmonary infarction may occur if the pulmonary venous pressure is
elevated or the bronchial arterial supply to a region is deficient for some
reason. The cone-shaped area of pulmonary infarction has been called a
Hampton’s hump (Figure 4-68 A) and is named after the person who originally
described it. An area of radiolucency, corresponding to diminished pul-monary
vascularity distal to a pulmonary embolism, is oc-casionally seen and is called
the Westermark sign. There may also be an increase in the size of the pulmonary
artery proximal to a large central pulmonary embolus (Fleischner sign).
Two imaging modalities are widely
used in the evalua-tion of a patient with suspected pulmonary embolism:
radionuclide perfusion scan and chest CTA. The radionu-clide perfusion scan may
be the more appropriate exami-nation in the patient with a normal chest
radiograph and no preexisting cardiac or pulmonary disease. In the pa-tient
with an abnormal chest radiograph, or preexisting cardiopulmonary disease, the
V/Q scan is more likely to be interpreted as “indeterminate” and a chest CT
becomes the preferred imaging modality. The chest CT also has the ad-vantage of
demonstrating unsuspected abnormalities, such as pericardial effusion, emphysema,
esophagitis, or aortic dissection, which could be responsible for the patient’s
chest pain or dyspnea.
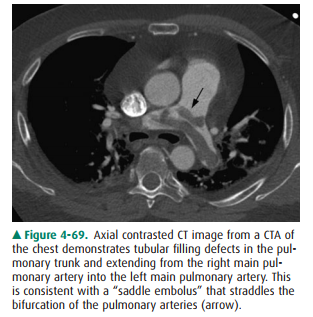
On chest CTA, thromboemboli are
visible as filling defects within the contrast-filled pulmonary arteries. These
are typi-cally several centimeters long and often are seen draped across the
bifurcation of an artery (saddle emboli) (Figure 4-69). In patients with acute
pulmonary embolism, the filling defects are seen within the center of the
arterial lumen, al-though they may also completely occlude the artery. In
pa-tients with chronic pulmonary embolism, the filling defects are more likely
to be found against the wall of the artery. Cal-cification within the thrombus
also confirms the chronic na-ture of the thrombus.
There will be some patients in whom
the diagnosis of pul-monary embolism remains uncertain after either a V/Q scan
or a chest CTA. These examinations can be inadequate for a number of both
technical and clinical reasons. The chest CTA can be difficult to interpret
unless the patient is able to sus-pend respiration for the duration of the
scan. Fortunately, helical CT scans are able to scan the entire thorax in under
20 seconds. Many patients with severe dyspnea, however, are unable to achieve
this. Pulmonary angiography can be ob-tained to further evaluate the pulmonary
arterial circulation when either the V/Q scan or chest CTA is nondiagnostic.
Related Topics