Chapter: Basic Radiology : Radiology of the Chest
Exercise: Diffuse Lung Opacities
EXERCISE 4-4.
DIFFUSE LUNG OPACITIES
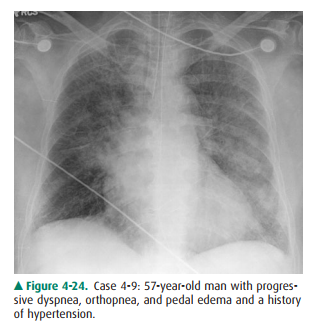
4-9. Which of the
following best describes the chest radi-ograph in Figure 4-24?
A.
Alveolar pulmonary edema
B.
Interstitial pulmonary edema, and small bilateral pleural
effusions
C.
Unilateral interstitial disease
D.
Oligemia in the right lung
Radiologic Findings
4-9. Frontal chest
radiograph (Figure 4-24) shows mild enlargement of the heart and indistinct
vascularity, particularly at the lower lungs. Interlobular septallines are
visible adjacent to both lower costophrenic angles. (B is the correct answer to
Question 4-9)
Discussion
Pulmonary edema can be divided
into two major categories: cardiogenic edema and noncardiogenic edema.
Cardiogenic edema occurs as a result of elevation of pulmonary capillary
pressure, which is usually due to pulmonary venous hyper-tension.
Noncardiogenic edema occurs as a result of disor-ders that increase pulmonary
capillary permeability. With both types of edema, there is a net movement of
fluid out of the microvasculature and into the pulmonary interstitium and
alveoli. The most common cause of pulmonary edema is left ventricular failure,
which may be due to atherosclerotic coronary artery disease, mitral or aortic
valvular disease, my-ocarditis, or cardiomyopathy. Cardiogenic edema is
preceded by pulmonary venous hypertension, which is associated with
redistribution of pulmonary blood flow from dependent re-gions of the lung to
nondependent regions. In the erect patient, the radiographic sign of this
redistribution is an increase in size of vessels in the upper lungs and a
decrease in the caliber of pulmonary vessels in the lung bases.
Radiographically, it is often difficult to distinguish pulmonary arteries from
pul-monary veins, but for purposes of determination of flow redis-tribution,
the distinction is ignored and multiple vessels are measured at equal distances
from the hilum or chest wall.
When seen end-on, normal
bronchoarterial bundles may appear as adjacent circles of equal diameter, with
the artery opaque and the bronchus lucent. The pulmonary arteries andbronchi
are located together in the same interstitial space and arborize adjacent to
each other. The pulmonary veins return blood to the heart in a separate
interstitial space and have a slightly different arborization pattern. As the
pulmonary venous pressure increases, fluid leaks from the pulmonary capillaries
into the adjacent interstitium. This interstitial pul-monary edema may be
identified by peribronchial cuffing, in-distinctness of the perivascular
margins, perihilar haziness, and thickening of the interlobular septa and
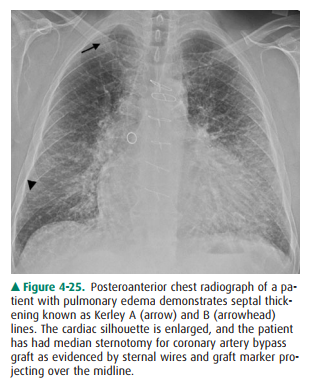
interlobar fis-sures. Septal thickening results in Kerley A (arrow) and Kerley
B (arrowhead) lines on chest radiograph (Figure 4-25). As the pulmonary
capillary pressure increases further, fluid spills into the alveoli, producing
a symmetrical appearance of air-space filling that is predominantly perihilar
(central) and basilar in distribution. Cardiogenic edema is greatest in
de-pendent regions of the lungs. In supine patients, the depend-ent regions are
the posterior segments of the upper lobes, and the superior and posterior basilar
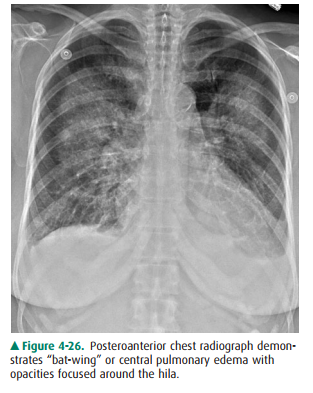
segments of the lower lobes. The central pattern of pulmonary edema has been
called “bat-wing” edema (Figure 4-26). As the pulmonary edema worsens, the
pulmonary and pleural lymphatics clear fluid from the lungs, and pleural
effusions will develop. In conges-tive heart failure, the pleural effusions are
generally small to moderate in size, and there is typically more fluid within
the right pleural space than the left. Isolated left pleural effusion is
unlikely to be due to congestive heart failure. In cardiogenic edema, the heart
size will be increased. The cardiothoracic ratio is a guide to determining
cardiac enlargement. The transverse dimension of the heart is divided by the
transverse diameter of the thorax at the same level. When the cardio-thoracic ratio
is greater than 0.5, cardiomegaly is often (but not always) present. When
possible, both the PA and lateral projections should be used to determine
cardiac volume. Cardiomegaly may be more readily recognized when com-parison is
made with prior radiographs. Comparison re-quires a similar depth of
inspiration and similar positioning of the patient (AP versus PA, supine versus
erect).
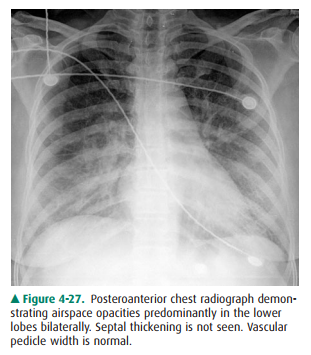
Noncardiogenic edema (Figure 4-27),
or “capillary leak” edema, may be due to a number of conditions, including
adult respiratory distress syndrome, fat embolism, amniotic fluid embolism,
drug overdose, near drowning, and acute air-way obstruction. The cause of
pulmonary edema in patients with intracranial injury or tumor (neurogenic
pulmonary edema) is uncertain. Similarly, the etiology of high-altitude
pulmonary edema is incompletely understood. The common radiographic findings in
noncardiogenic edema are symmet-ric, diffuse areas of airspace filling that is
often patchier in appearance and more peripheral in distribution. The heart
size is usually normal; pleural effusions and septal lines are typically
absent. The vascular pedicle is of normal width.
Renal failure and volume overload
may result in pul-monary edema, which may be chronic. When the degree of edema
is small to moderate, patients are often reasonably well compensated and are
able to carry out many activities of daily living.
Related Topics