Chapter: Basic Radiology : Radiology of the Chest
Exercise: Pleural Effusion
EXERCISE 4-13.
PLEURAL EFFUSION
4-21. Which of the
following radiographic signs generally does not suggest the presence of pleural
effusion?
A.
Meniscus-shaped opacity in a posterior cost-ophrenic angle on
the lateral projection
B.
Biconvex lens-shaped opacity projecting in the midthorax on the
lateral projection
C.
Fluid levels that have the same lengths on the PA and lateral
views in a hemithorax
D.
Homogenous increased density in a hemithorax with preservation
of the vascular shadows in the lungs
E.
Separation of the gastric air bubble from the infe-rior lung
margin by more than 2 cm
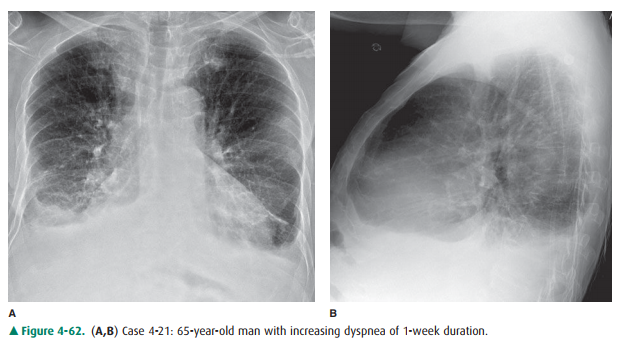
Radiologic Findings
The frontal chest radiograph
(Figure 4-62 A) shows opacity at the lower hemithorax bilaterally, which has a
concave bor-der curving upward laterally adjacent to the chest wall. The
overall lung volume is low in both the right and left lungs. There is
separation of the gastric bubble from the inferior margin of the lung by
several centimeters. On the lateral ex-amination (Figure 4-62 B), the opacities
obscure the poste-rior heart margin and have a margin curving slightly upward
to the posterior chest wall. Neither hemidiaphragm can be followed posteriorly
to the chest wall. The findings are those of bilateral pleural effusions (C is
the correct answer to Question 4-21).
Discussion
The visceral pleura is the outer
lining of the lung, and the parietal pleura is the lining of the chest cavity.
Normally, these surfaces are smooth and are separated by a minimal amount of
pleural fluid. This provides a nearly friction-free environment for movement of
the lung within the thorax. The pleural space, therefore, is a potential space
that, in the normal individual, contains no more than 3 to 5 mL of pleu-ral
fluid. Fluid may accumulate within the pleural space as a result of conditions
that (1) increase pulmonary capillary pressure, (2) alter thoracic vascular or
lymphatic pathways, alter pleural capillary
or lymphatic permeability, or affect diaphragmatic
peritoneal and pleural surfaces. Pleural effusions are usually approached
clinically according to whether the effusion develops because of alter-ations
of the Starling equation, which controls fluid flow and maintenance in body
compartments, or whether the pleura is affected primarily by a disease process.
Processes resulting from alterations of the Starling equation include
congestive heart failure, hypoproteinemia, fluid overload, liver failure, and
nephrosis. These effusions are usuallytransudates (clear or pale yellow,
odorless fluid without ele-vation of the ratios of pleural fluid to serum
protein and lac-tate dehydrogenase [LDH]). Processes that alter pleural
capillary or lymphatic permeability include infection, in-flammation, pulmonary
embolism, and neoplasms. These effusions are usually exudates (clear, pale
yellow or turbid, bloody, brownish fluid; pleural fluid protein: serum protein
greater than 0.5; and pleural fluid LDH:serum LDH greater than 0.6). Enlarged
lymph nodes or masses within the hila or mediastinum may obstruct lymphatic
fluid flow and cause pleural exudates. Abdominal conditions that may produce
pleural effusions include pancreatitis, subphrenic abscesses, liver abscesses, ovarian
tumors, peritonitis, and ascites.
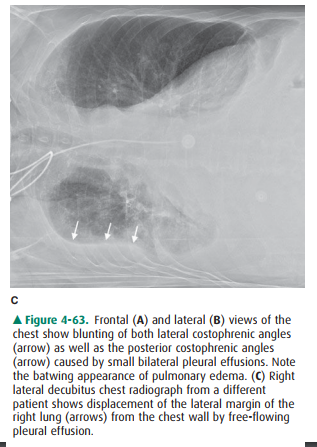
The most common radiographic sign
of pleural effusion is pleural meniscus. The volume of fluid necessary to
pro-duce a pleural meniscus within a costophrenic angle varies from individual
to individual. Approximately 100 mL of pleural fluid will cause appreciable
blunting of the posterior costophrenic angle on the lateral view (Figure 4-63
A), and 200 mL will cause blunting of the lateral costophrenic angle on the PA
projection in an upright patient (Figure 4-63 B). A lateral decubitus chest
radiograph, with the side containing the pleural effusion placed down
(dependent), will demon-strate even smaller amounts of free-flowing pleural
effusions (Figure 4-63 C). Each millimeter of thickness of pleural fluid in the
lateral decubitus projection corresponds to approxi-mately 20 mL of pleural
fluid. Large pleural effusions may usually be aspirated without guidance other
than the chest radiograph. Small effusions are more difficult to aspirate and,
if thoracentesis is planned, additional imaging guidance with ultrasonography
or CT may be used. The effusion may simply be marked and aspirated by the
clinical physician, or the effusion may be aspirated by a radiologist. If
thoracente-sis is attempted and fails for a large pleural effusion, it may be
loculated and further imaging guidance is usually helpful.
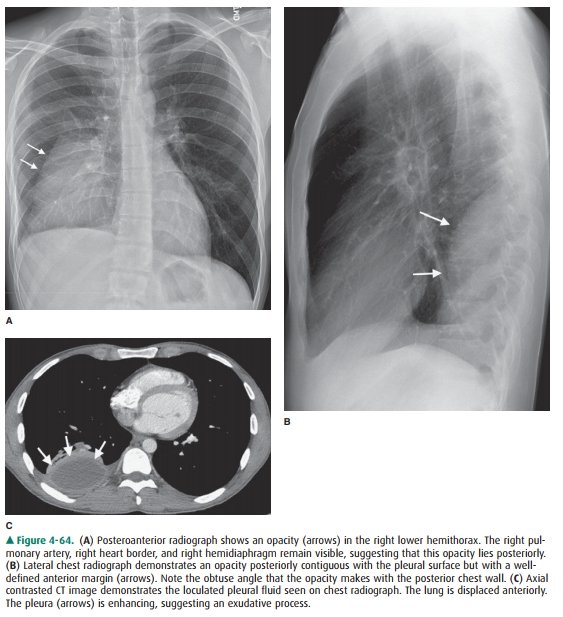
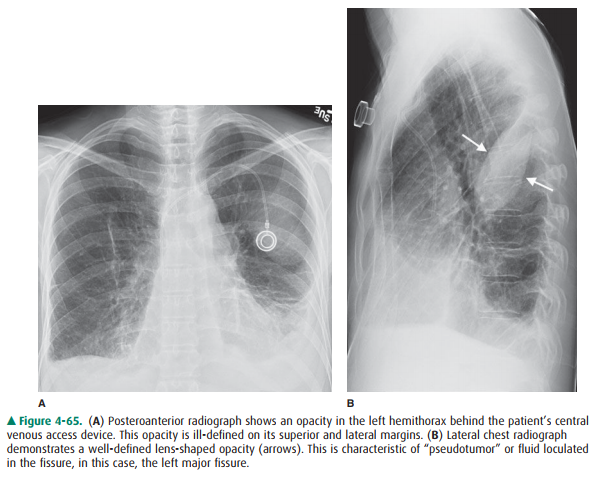
When pleural adhesions develop,
fluid in the pleural space becomes loculated (Figure 4-64 A–C) and may be
trapped in nondependent areas of the thorax. The appearance of pleuralfluid may
change and, rather than taking a meniscus shape, may assume the shape of a
convex margin away from the chest wall. If air is introduced in the pleural
space by penetra-tion of the chest wall, or if fluid is trapped in the
fissures, it will assume a biconvex lens shape (Figure 4-65). If a
bron-chopleural fistula develops, the patient will have a hydrop-neumothorax
that may be recognized by air-fluid levels of different lengths on the PA and
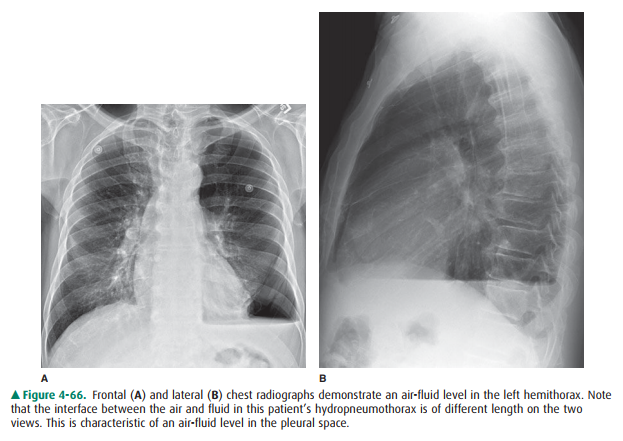
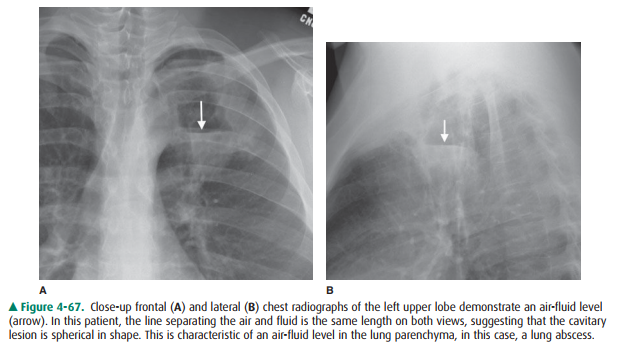
lateral chest radiographs (Figure 4-66). When cavities develop in the lung, the
fluid levels are usually of the same length (Figure 4-67).
Related Topics