Chapter: Psychology: Treatment of Mental Disorders
Psychological Treatments: Behavioral Approaches
Behavioral Approaches
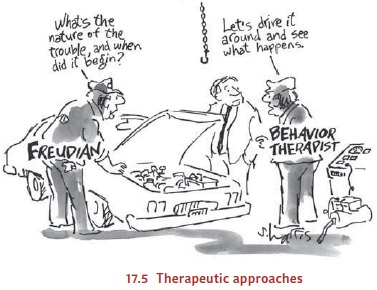
Like
the humanistic therapies, behavior therapies emerged in part as a reaction to
the Freudian tradition of psychoanalysis (Figure 17.5). But while the humanists
regarded psychoanalysis as too mechanis-tic, the behavior theorists,
ironically, offered exactly the opposite crit-icism; they regarded
psychoanalysis as too loose and unscientific.
Behavior
therapists focus on overt behavior rather than uncon-scious thoughts and
wishes, which they regard as hard to define and impossible to observe. The
patient’s behaviors, in other words, are not regarded as “symptoms” through
which one can identify and then cure an underlying illness. Instead, these
therapists view the maladaptive behaviors themselves as the problem to be
solved. These behaviors, in turn, are, from a behaviorist’s perspective, simply
the results of learning—albeit learning that led the person to undesired or
undesirable behaviors.
The
remedy, therefore, involves new learning, in order to replace old habits with
more effective or adaptive ones. For this purpose, the therapeutic procedures
draw on the principles of behavior change that have been well documented in the
laboratory— classical conditioning, operant conditioning, and modelling.
CLASSICAL
CONDITIONING TECHNIQUES
To see how behavior therapy proceeds, consider the treatment for specific phobias (Emmelkamp, 2004; Wolpe & Plaud, 1997). According to behavior therapists, the irra-tional fears that characterize these phobias are simply classically conditioned responses, evoked by stimuli that have become associated with a truly fearful stimulus. The way to treat these phobias, therefore, is to break the con-nection between the phobic stimuli and the associated fears, using a technique akin to the extinction procedures that are effective in diminishing conditioned responses in the laboratory.
One
early version of this procedure is the technique originally known as systematic
desensitization, now referred to as exposure
therapy. Here, the therapist seeks not only to break the connection between
the phobic stimulus and the fear response but also to create a new connection
between this stimulus and a different response, one that is incompatible with
fear and will therefore displace it (Figure 17.6). The new response is usually
deep muscular relaxation, and the patient is taught a relaxation technique,
typically through meditation-like exercises, before the formal therapy begins.
Then, once the patient has learned to relax deeply on cue, the goal is to
condi-tion this relaxation response to the stimuli that have been evoking fear.
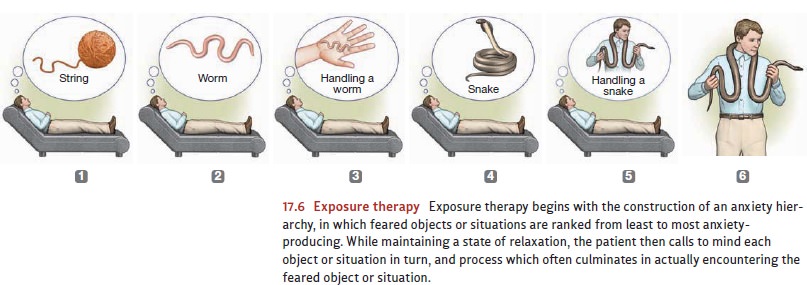
To
begin the therapy, the patient constructs an anxiety hierarchy, in which feared
sit-uations are identified and then ranked from least to most anxiety
provoking. This hier-archy is then used to set the sequence for therapy. The
patient starts out by imagining the first scene in the hierarchy (e.g., being
on the first floor of a tall building) while in a state of deep relaxation. He
will stay with this scene—imagining and relaxing—until he no longer feels any
anxieties. After this, he imagines the next scene (perhaps look-ing out a
fourth-floor window in the building), and this scene, too, is thoroughly
“counter-conditioned,” meaning that the old link between the scene and an
anxiety response is broken, and a new link between the scene and a relaxation
response is forged. The process continues, climbing up the anxiety hierarchy
until the patient finally can imag-ine the most frightening scene of all
(leaning over the railing of the building’s observa-tion tower, more than 100
floors above the ground) and still be able to relax.
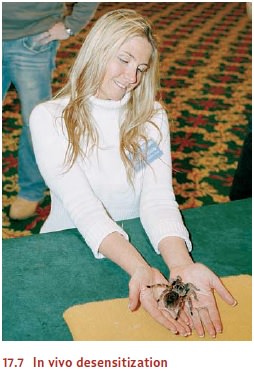
Sometimes
this imagined exposure is sufficient to treat the phobia, but often patients
need to extend the graduated exposure to the real world—for example, actu-ally
visiting a tall building rather than merely thinking about one. This process,
called in vivo desensitization, may
take place with the therapist present or may use guidedhomework assignments
(Figure 17.7; Craske, 1999; Goldfried & Davison, 1994). In addition,
interactive computer graphics now provide yet another option: exposing the
patient to a virtual-reality version of the frightening stimulus, which seems
to be another way to extend and strengthen the desensitization procedure
(Figure 17.8; see, for example, Emmelkamp et al., 2002). However the feared
stimulus or situation is presented, exposure is a key ingredient in therapeutic
success.

OPERANT
CONDITIONING TECHNIQUES
A
second set of behavioral techniques is based on the principles of instrumental
or operant conditioning. These techniques aim to change behavior through
reinforcement by emphasizing the relationship between acts and consequences.
An
example of this approach is the use of token
economies in hospital psychiatric wards. In these settings, patients earn
the tokens through various helpful or healthy behaviors such as making the bed,
being neatly dressed, or performing ward chores. They can then exchange tokens
for desirable items, such as snacks or the chance to watch TV. In this fashion,
the patient is systematically rewarded for producing desirable behaviors and is
not rewarded for producing undesirable ones.
As
in the learning laboratory, the reinforcement contingencies can then be
gradu-ally adjusted, using the process known as shaping. Early on, the patient
might be rein-forced merely for getting out of bed; later, tokens might be
awarded only for getting out of bed and walking to the dining hall. In this
fashion, the patient can be led, step-by-step, to a higher level of
functioning. The overall effects of this technique are that the patients become
less apathetic and the general ward atmosphere is much improved (Higgins,
Williams, & McLaughlin, 2001).
Other
reinforcement procedures can be useful in individual behavior therapy as part
of contingency management. In this
procedure, the person learns that certain behav-iors will be followed by strict
consequences (Craighead, Craighead, Kazdin, & Mahoney, 1994). For example, a
child who is oppositional and defiant can be presented with a menu of “good
behaviors” and “bad behaviors,” with an associated reward and penalty for each.
Being a “good listener” can earn the child the chance to watch a video,
cleaning up her room every day can get her a dessert after dinner, and so
forth, whereas talking back to Mom or making a mess may result in an early
bedtime or a time-out in her room. The idea is not to bribe or coerce the child
but to show her that her actions can change the way people react to her.
Ideally, her changed behavior will result in a more positive social environment
that will eventually make explicit rewards and pun-ishments unnecessary.
These operant techniques have been applied to a number of mental disorders. In one study, parents spent 40 hours a week attempting to shape the behavior of their uncom-municative 3-year-olds who had autism (Lovaas, 1987). By first grade, more than half of the children were functioning successfully in school, and these treatment gains were still evident four years later (McEachin, Smith, & Lovaas, 1993). In a group of 40 compara-ble children who did not receive this intervention, only one child showed comparable improvement by first grade. Others have applied this technique to other serious mental disorders such as mental retardation, with positive results (Reid, Wilson, & Faw, 1991).
MODELING TECHNIQUES
One
last (and powerful) technique for the behavior therapist is modeling, in which someone learns new
skills or changes his behavior by imitating another person (Figure 17.9).
Sometimes, the therapist serves as the model, but this need not be the case.
Therapy with children, for example, may draw on young “assistants” (children roughly
the same age as the child in therapy) who work with the therapist and model the
desired behaviors or skills.
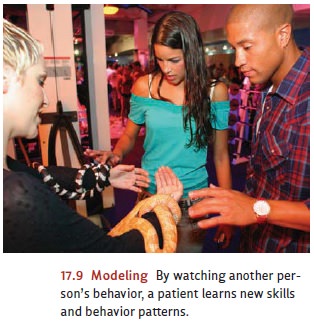
Modeling
is not limited to overt behaviors; a therapist can also model a thought process
or a decision-making strategy. In some forms of therapy, the therapist “thinks
out loud” about commonplace decisions or situations, in this way providing a
model for how the patient should consider similar settings (Kendall, 1990;
Kendall & Braswell, 1985). Likewise, modeling can be used for emotional
responses, so that, for example, the therapist can model fearlessness in the
presence of some phobic stimulus and in this fashion diminish the phobia
(Bandura, 1969, 2001).
Modeling
can also be supported by vicarious reinforcement, a procedure in which the patient
sees the model experience some good outcome after exhibiting the desired
behavior or emotional reaction. Like other forms of reinforcement, vicari-ous
reinforcement seems to increase the likelihood that the person in therapy will
later produce the desired behavior or reaction.
Related Topics