Chapter: Psychology: Treatment of Mental Disorders
Current Treatments for Mental Disorders
Current Treatments for Mental Disorders
As
we saw, mental disorders typically involve many factors, some biolog-ical and
some rooted in a person’s circumstances. Different treatments target different
aspects of this network of interrelated causes. Psychological treatments aim to
alter psychological and environmental processes via “talk therapy.” Biomedical
treatments seek to alter underlying biological processes directly, often
through medication or neurosurgery.
For
convenience, we will use this distinction between psychological and biomedical
treatments. However, this shorthand does risk introducing some confusion. If we
focus narrowly on the overt steps in treatment, we can distinguish psychological
approaches (talking to a patient, perhaps leading her to new insights or new
beliefs) from biomedical approaches (perhaps prescribing a pill for the patient
to take twice a day). However, if we broaden our focus, the distinction between
the psychological and the biological becomes less clear-cut. After all,
psychological processes are the prod-ucts of functioning brains—and so changes
in people’s psychology necessarily involve changes in their brain. Hence
psychological treatments have biological effects. Conversely, biomedical
treatments may in many cases work by altering a person’s thought processes or
shifting a person’s mood; for this reason, the biological treatments often need
to be under-stood in “psychological” terms. In either direction, therefore, a
distinction between “psy-chological” and “biological” treatments is somewhat
artificial (Kumari, 2006). In addition, as we will see, contemporary treatments
often combine talk therapy with med-ication, further blurring the line between
psychological and biological treatment.
That
said, it is still useful to distinguish between treatments that emphasize
psycho-logical approaches and those that emphasize biological approaches, and
this leads us to ask: How does a practitioner decide which emphasis is best in
a given case? The answer depends on the illness and our understanding of its
causes. If the illness seems shaped primarily by environmental causes (such as
a hostile family environment) or by the person’s perceptions and beliefs, then
a psychological intervention may be best— helping the person to find ways to
cope with (or change) the environment, or persuad-ing the person to adopt new
beliefs. If the illness seems shaped primarily by some biological dysfunction
(perhaps an overreactive stress response, for example, or a short-age of some
neurotransmitter), then a biomedical intervention may be preferable.
However,
these points are at best rough rules of thumb. In many cases, there may be no
direct correspondence between what triggers a disorder (a specific biological
dysfunction or some life problem) and the nature of the treatment. Some
problems arising from a difficult situation are best treated medically; some
problems arising from a biological dysfunction are best treated with psychotherapy.
In choosing a form of therapy, practitioners must focus on what works, rather
than focusing exclusively on how the disorder arose.
TREATMENT PROVIDERS
We
will have a great deal to say about these two broad emphases in treatment—the
psychological and the biological—and the specific ways that treatment unfolds.
Before we turn to these details, let’s consider the providers and recipients of
these treatments.
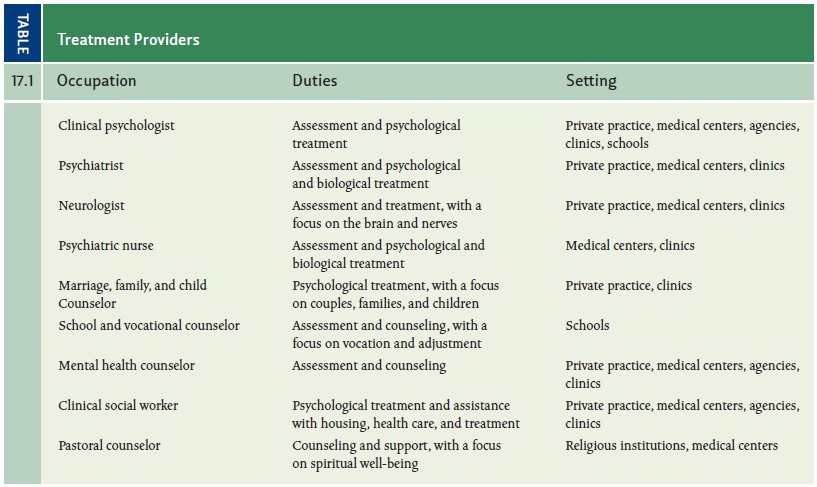
An
extraordinarily wide range of professionals and non-professionals provide
treat-ments for mental disorders. Individuals licensed to provide psychological
treatments include clinical psychologists; psychiatrists; psychiatric nurses;
marriage, family, and child counselors; school and vocational counselors;
mental health counselors; and clinical social workers. Psychological
interventions are also administered by individu-als with varying degrees of
psychological training including pastoral counselors, reli-gious leaders, and
paraprofessionals. A description of each of these treatment providers is given
in Table 17.1.
Surprisingly,
more experienced providers are not always more effective than less experienced
providers (McFall, 2006), and even professional credentials are not
neces-sarily a good predictor of therapeutic success (Blatt, Sanislow, Zuroff,
& Pilkonis, 1996). These findings suggest that who the therapist is, what
he or she does, and how well this matches the patient’s needs may be far more
important than the therapist’s level of experience or the degrees he has
earned. Also crucial is the quality of the rapport
the therapist establishes with the patient—whether the patient respects and
trusts the therapist and feels comfortable in the therapeutic setting. This
rapport, too, is often more important than the therapist’s credentials or type
and degree of training.
Psychological
treatments can be administered either with or without a license (with the
license usually given by the state in which the therapist is practicing). In
clear con-trast, the administration of biomedical treatments does require a
license. Here too, however, there are many different providers, including
psychiatrists, neurologists, and psychiatric nurses. In fact, this list has
been growing, with some jurisdictions now per-mitting “prescription privileges”
for clinical psychologists—that is, allowing people with Ph.D.s to write
prescriptions, a privilege that used to be reserved for people with medical
degrees.
TREATMENT RECIPIENTS
People
seek treatment for a wide variety of reasons. Some seek relief from the pain
and dysfunction associated with a diagnosable mental disorder. Others suffer
with subsyn-dromal disorders—versions
of mental disorders that don’t meet the criteria for diag-nosis but that may
nonetheless cause significant problems (Ratey & Johnson, 1997). Others have
neither a full-fledged nor a sybsyndromal disorder but instead seek help with
feelings of loss, grief, or anxiety, with relationship difficulties, or with
confusion about a major life decision. Still others seek therapy in order to
live happier and more fulfilled lives.
Just
as important is a listing of people who might benefit from therapy but don’t
seek it. Surveys reveal that in the United States, only about 40% of those with
clinically significant disorders (such as depression, anxiety, or substance use
disorders) had received treatment in the past year (Wang, Bergulund, et al.,
2005). Women are more likely than men to seek treatment (Addis & Mahalik,
2003; Wang, Berglund, et al., 2005), and European Americans are more likely to
seek treatment than Asian Americans and Hispanic Americans (Sue & Lam,
2002; Wang, Berglund, et al., 2005).
There
is yet another (and very large) group of people who might benefit from therapy
but cannot get it. According to the World Health Organization, roughly 450
million people worldwide suffer from various mental disorders, and the clear
majority live in developing countries—90% of these people have no access to
treat-ment (Miller, 2006b). Access is also an issue in developed countries.
Many forms of mental illness are more common among the poor, but the poor are
less likely to have insurance coverage that will make the treatment possible
(Wang, Lane, et al., 2005).
CULTURAL CONSIDERATIONS
Some
of the problems just described could—in theory—easily be solved. We could train
more therapists and open more clinics so that treatment would be available to
more people. We could improve insurance coverage or arrange for alternative
forms of financing. These steps, however, would not be sufficient, because
there is still another factor that limits the number of people who can benefit
from therapy: the limited availability of culturally
appropriate therapy and culturally
competent therapists.
A
therapist shows cultural competence
by understanding how a patient’s beliefs, values, and expectations for therapy
are shaped by his cultural background (Sue, 1998). A therapist with this
understanding can modify the goals of therapy to conform to the patient’s values
(Hwang, 2006). For example, many Asian cultures emphasize formal-ity in all
their affairs. Social roles within these cultures are often clearly defined and
tend to be structured largely by age and sex, such that a father’s authority is
rarely chal-lenged within the family. Growing up in such a culture may play an
important part in shaping the values a patient brings to therapy. A therapist
insensitive to these values risks offending the patient and endangering the
therapy. Similarly, a therapy that emphasizes individual autonomy over family
loyalties might inadvertently violate the patient’s cultural traditions and so
be counterproductive.
Cultural
sensitivity also includes other issues. For example, therapists who expect
their patients to take responsibility for making changes in their lives may be
ineffective with patients whose cultural worldview stipulates that important
events are caused by factors such as fate, chance, or powerful others.
Likewise, practitioners who consider psychotherapy a secular endeavor would do
well to remember that in many cultures, any kind of healing must acknowledge
the patient’s spirituality.
Attention
to such cultural differences may also be valuable for another reason: it’s
possible that the Western world can learn something about the treatment of
mental disorders from the cultures in developing countries. For example, the
long-term prog-nosis for schizophrenia is considerably better in developing
countries than it is in the United States (Thara, 2004). Patients with schizophrenia
in India, as one illustration, show far more remission of symptoms and fewer
relapses than patients with schizo-phrenia in the United States and often
recover enough to hold a full-time job, marry, and otherwise lead reasonably
normal lives.
Why
is this? Some suggest that physicians in the United States rely too much on
medication in treating schizophrenia and too little on interventions that
emphasize job training and a supportive social network. The opposite is the
case in India, where med-ication is often not available and
institutionalization is usually not an option. Indeed, it is estimated that
roughly 99% of individuals with schizophrenia live with their fam-ilies in
India, compared with 15 to 25% in the United States (Thara, 2004). Of course,
the style of treatment in the United States is encouraged by many factors,
including families that may want to distance themselves from the patient and
insurance compa-nies that will reimburse patients for psychotropic drugs but
hesitate to pay for social programs.
It
seems, then, that cultural competence needs to be broadly understood. It
includes the need for Western-style practitioners to be alert to the cultural
background (and so to the assumptions, beliefs, and values) of their patients.
But it also includes an open-ness to the possibility that the style of treating
mental illness in other cultures may, for some disorders, be preferable to the
methods used in the developed countries. We need to keep these points in mind
as we turn to a consideration of what the various forms of treatment involve.
Related Topics