Chapter: Modern Pharmacology with Clinical Applications: Pharmacological Management of Chronic Heart Failure
Propranolol
CLASS II
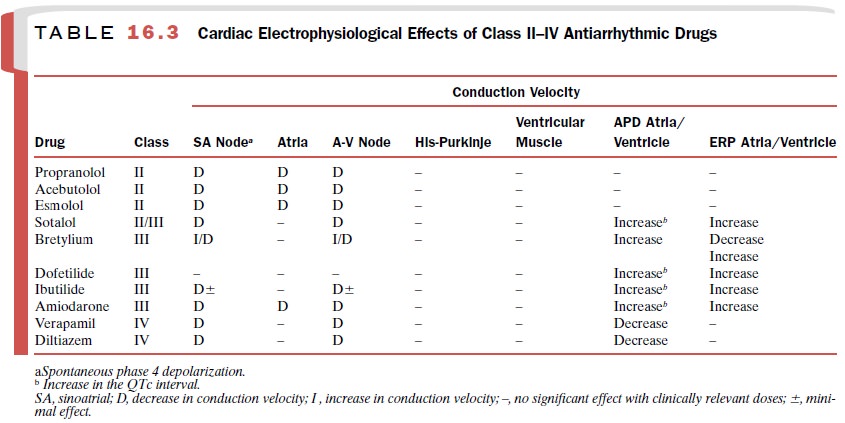
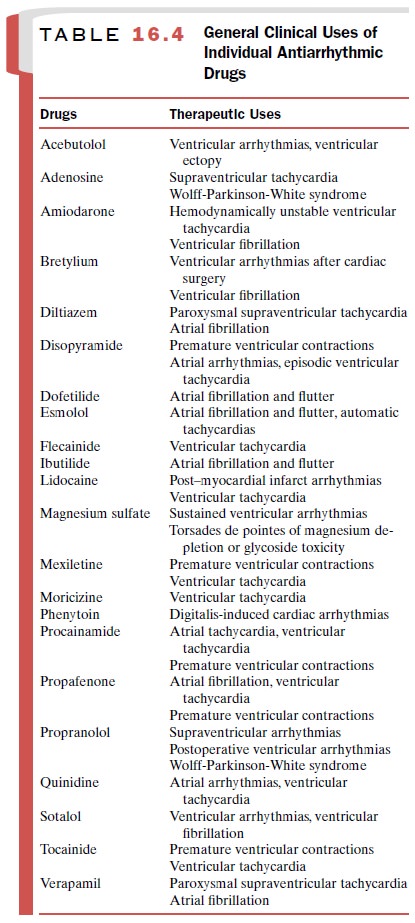
Table 16.3 summarizes the
cardiac electrophysiological effects of class II, III, and IV agents, and Table16.4
sum-marizes the actions of the β-receptor blocking agents
Bear in mind the complete spectrum of cardiovascular effects of these
agents when prescribing their use. For example, while patients with a normally
functioning cardiovascular system may tolerate adrenergic blockade of the
heart, patients with compensated heart failure, who depend on adrenergic tone to
maintain an adequate cardiac output, may un-dergo acute congestive heart
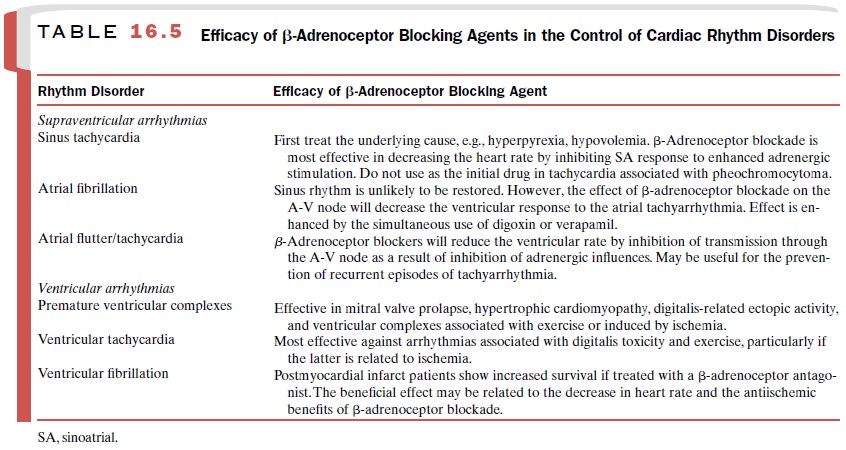
failure if prescribed any of the class II drugs. Table 16.5 summarizes the
clinical use of the β-adrenoceptor blocking drugs in the treatment of cardiac
arrhythmias.
Propranolol
Propranolol (Inderal) is the prototype β-blocker . It
decreases the effects of sympathetic stimulation by competitive binding to β-adrenoceptors.
Electrophysiological Actions
Propranolol has two separate
and distinct effects. The first is a consequence of the drug’s β-blocking properties
and the subsequent removal of adrenergic influences on the heart. The second is
associated with its direct myo-cardial effects (membrane stabilization). The
latter ac-tion, especially at high clinically employed doses, may account for
its effectiveness against arrhythmias in which enhanced β-receptor stimulation
does not play a significant role in the genesis of the rhythm disturbance.
Sinoatrial Node
Propranolol slows the
spontaneous firing rate of nodal cells by decreasing the slope of phase 4
depolar-ization.
Atrium
Propranolol has local
anesthetic properties and ex-erts actions similar to those of quinidine on the
atrial membrane action potential. Membrane responsiveness and action potential
amplitude are reduced, and ex-citability is decreased; conduction velocity is
reduced. Because these concentrations are similar to those that produce β-blockade, it is impossible
to determine whether the drug acts by specific receptor blockade or via a
membrane-stabilizing effect.
A-V Node
The depressant effects of
propranolol on the A-V node are more pronounced than are the direct depres-sant
effects of quinidine. This is due to propranolol’s dual actions of β-blockade and direct
myocardial de-pression. Propranolol administration results in a de-crease in
A-V conduction velocity and an increase in the A-V nodal refractory period.
Propranolol does not display the anticholinergic actions of quinidine and other
antiarrhythmic agents.
His-Purkinje System and Ventricular Muscle
Propranolol decreases Purkinje fiber membrane re-sponsiveness and reduces action potential amplitude. His-Purkinje tissue excitability also is reduced. These changes result in a decrease in His-Purkinje conduction velocity. However, these electrophysiological alter-ations are observed at propranolol concentrations in excess of those normally used in therapy. The most striking electrophysiological property of propranolol at usual therapeutic concentrations is a depression of catecholamine-stimulated automaticity.
Electrocardiographic Changes
Propranolol prolongs the PR
interval but does not change the QRS interval. It may shorten the QT interval.
Hemodynamic Effects
The blockade of cardiac β-adrenoceptors prevents or
reduces the usual positive inotropic and chronotropic actions of catecholamine
administration on cardiac sympathetic nerve stimulation. Blockade of β-receptors
prolongs systolic ejection periods at rest and during ex-ercise. Both
alterations tend to increase myocardial oxygen consumption. However, these
alterations are offset by factors that tend to reduce oxygen consump-tion, such
as decreased heart rate and decreased force of contraction. The decrease in
oxygen demand pro-duced by a decrease in heart rate and a decrease in force of
contraction is usually greater than the increase in oxygen demand that results
from increased heart size and increased ejection time. The net result is that
oxy-gen demand is decreased.
Pharmacokinetics
The pharmacokinetic
characteristics of propranolol:
Oral bioavailability : 30–40%
Onset of action : 1–2 hours
Peak response : 1.0–1.5 hours
Duration of action : 6–24
hours
Plasma half-life : 3–5 hours
Primary route of metabolism :
Hepatic
Primary route of excretion : Renal
Therapeutic serum
concentration : 0.02–1 μg /mL
Clinical Uses
Propranolol is indicated in the management of a variety of cardiac
rhythm abnormalities that are totally or par-tially due to enhanced adrenergic
stimulation. In se-lected cases of sinus tachycardia caused by anxiety,
pheochromocytoma, or thyrotoxicosis, β-blockade will reduce the spontaneous heart
rate.
Propranolol alone or in
conjunction with digitalis can help control the ventricular rate in patients
with atrial flutter or atrial fibrillation. Patients with supraventricular
extrasystoles and intermittent parox-ysms of atrial fibrillation may benefit
from β-receptor blockade with propranolol.
The arrhythmias associated
with halothane or cyclo-propane anesthesia have been attributed to the
interac-tion of the anesthetic with catecholamines, and they have been
suppressed by IV administration of 1 to 3 mg propranolol. An increase in
circulating catecholamines also has been observed in patients with acute
myo-cardial infarction and has been correlated with the de-velopment of
arrhythmias.
Clinically, tachyarrhythmias
associated with digitalis excess (including supraventricular and ventricular
ex-trasystoles) and ventricular tachycardia have been sup-pressed by
propranolol. Although propranolol is highly effective in the treatment of digitalis-induced
arrhyth-mias, phenytoin and lidocaine are preferred.
Long-term treatment with β-adrenoceptor blocking agents
is clearly associated with an increased rate of
survival in patients with
ischemic heart disease who have recovered from an acute myocardial infarction.
Propranolol is the drug of choice for treating patients with the congenital
long QT syndrome.
Adverse Effects
The toxicity associated with
propranolol is for the most part related to its primary pharmacological action,
inhi-bition of the cardiac β-adrenoceptors. In addition, propranolol exerts direct cardiac
depressant effects that become manifest when the drug is administered rapidly
by the IV route. Glucagon immediately reverses all cardiac de-pressant effects
of propranolol, and its use is associated with a minimum of side effects. The
inotropic agents amrinone (Inocor)
and milrinone (Primacor) provide
alternative means of augmenting cardiac contractile function in the presence of
β-adrenoceptor blockade .
Propranolol may also stimulate bron-chospasm in patients with asthma.
Since propranolol crosses the
placenta and enters the fetal circulation, fetal cardiac responses to the
stresses of labor and delivery will be blocked. Additionally, propranolol
crosses the blood-brain barrier and is associ-ated with mood changes and
depression. School difficul-ties are commonly associated with its use in
children. Propranolol may also cause hypoglycemia in infants.
Contraindications
Propranolol is
contraindicated for patients with de- pressed myocardial function and may be
contraindicated in the presence of digitalis toxicity because of the
possi-bility of producing complete A-V block and ventricular asystole. Patients
receiving anesthetic agents that tend to depress myocardial contractility
(ether, halothane) should not receive propranolol. Propranolol should be used
with extreme caution in patients with asthma.
Up-regulation of β-receptors
follows long-term therapy, making abrupt withdrawal of β-blockers dan-gerous
for patients with ischemic heart disease.
Related Topics