Chapter: Modern Pharmacology with Clinical Applications: Pharmacological Management of Chronic Heart Failure
Cardiac Electrophysiology: Automaticity
Automaticity
Automaticity can be defined
as the ability of a cell to al-ter its resting membrane potential toward the
excitation threshold without the influence of an external stimulus. The
characteristic feature of cells with automaticity is a slow decrease in the
membrane potential during dias-tole (phase 4) such that the membrane potential
reaches threshold (Figure 16.2). During phase 4 in these pacemaker cells, the
background potassium leak cur-rent decreases and an inward depolarizing current
(If) is
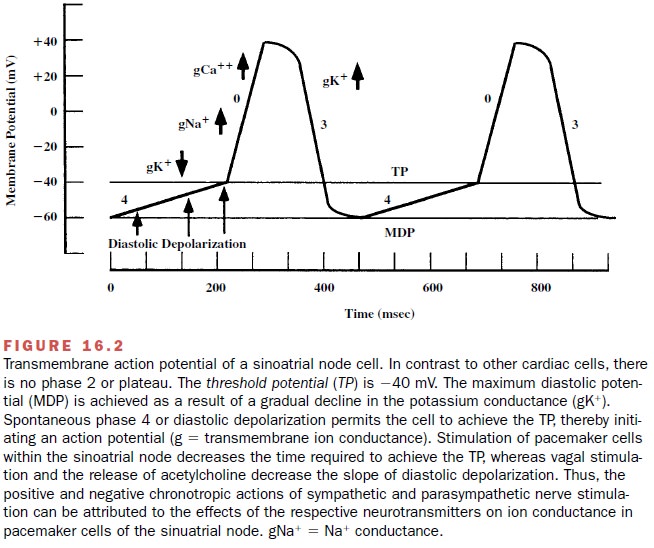
In combination,
this results in slow depolar-ization of the myocyte. If the membrane potential
de-polarizes above the threshold for the opening of ICa , an action
potential is generated.
Myocytes within the
sinoatrial node possess the most rapid intrinsic rate of automaticity;
therefore, the sinoatrial node serves as the normal pacemaker of the heart.
Specialized cells within the atria, atrioventricular (A-V) node, and
His-Purkinje system are capable of spontaneous depolarization, albeit at a
slower rate. The more rapid rate of depolarization of the sinoatrial nodal cells
normally suppresses all of the other cells with the potential for automaticity.
The other cells will become pacemakers
when their own intrinsic rate of depolariza-tion becomes greater than that of
the sinoatrial node or when the pacemaker cells within the sinoatrial node are
depressed. When impulses fail to conduct across the A-V node to excite the
ventricular myocardium (heart block), spontaneous depolarization within the
His-Purkinje system may become the dominant pacemaker maintaining cardiac
rhythm and cardiac output.
The rate of pacemaker
discharge within these spe-cialized myocytes is influenced by the activity of
both divisions of the autonomic nervous system. Increased sympathetic nerve
activity to the heart, the release of catecholamines from the adrenal medulla,
or the exoge-nous administration of adrenomimetic amines will cause an increase
in the rate of pacemaker activity through stimulation of β-adrenoceptors on the
pace-maker cells (Figure 16.3).
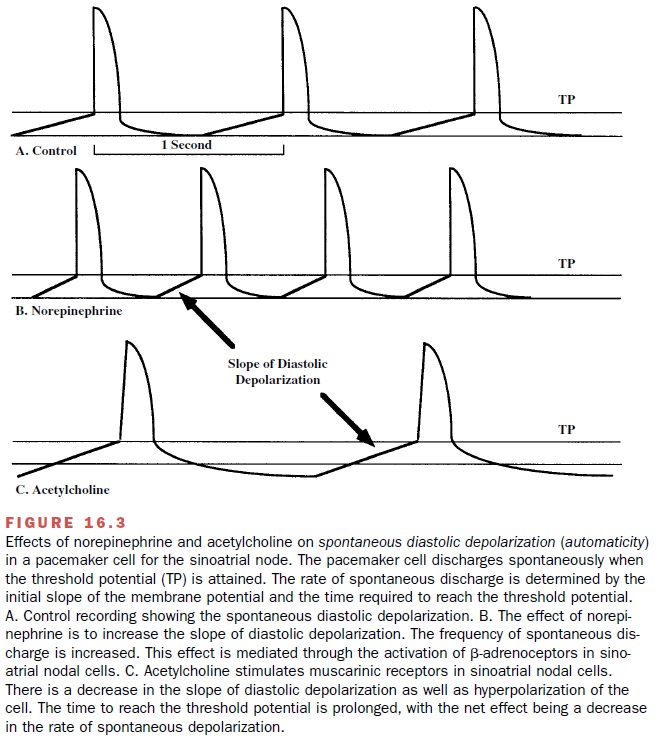
The parasympathetic nervous system, through the vagus nerve, inhibits the spontaneous rate of depolar-ization of pacemaker cells. The release of acetylcholine from cholinergic vagal fibers increases potassium con-ductance (gK+ ) in pacemaker cells, and this enhanced outward movement of K+ results in a more negative potential, or hyperpolarization, of the sinoatrial cells. Thus, during vagal stimulation, the threshold potential of the sinoatrial node pacemaker cells is achieved more slowly and the heart rate is slowed.
Related Topics