Chapter: Modern Pharmacology with Clinical Applications: Pharmacological Management of Chronic Heart Failure
Procainamide
Procainamide
Procainamide (Pronestyl, Procan SR) is a derivative of
the local anesthetic agent procaine. Procainamide has a longer half-life, does
not cause CNS toxicity at thera-peutic plasma concentrations, and is effective
orally. Procainamide is a particularly
useful antiarrhythmic drug, effective in the treatment of supraventricular,
ven-tricular, and digitalis-induced arrhythmias.
Electrophysiological Actions
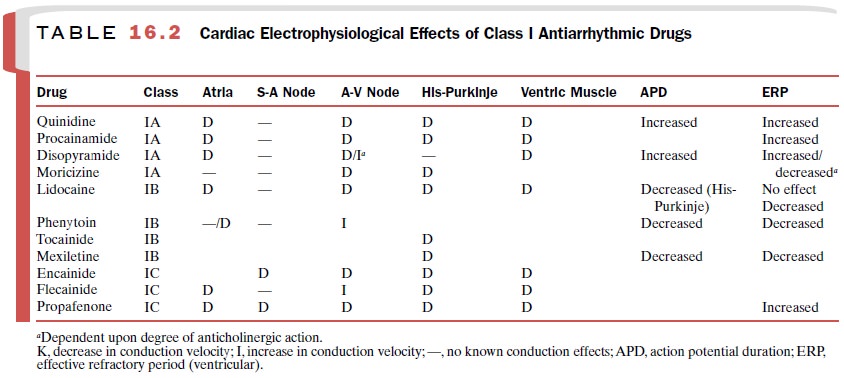
Table 16.2 describes the
direct, indirect, and net actions of procainamide on cardiac electrophysiology.
Hemodynamic Effects
The hemodynamic alterations
produced by pro-cainamide are similar to those of quinidine but are not as
intense. Alterations in circulatory dynamics vary ac-cording to the
cardiovascular state of the individual. The hypotensive effects of procainamide
are less pro-nounced after intramuscular administration and seldom occur after
oral administration.
Pharmacokinetics
The pharmacokinetic
characteristics of procainamide:
Oral bioavailability : 75–95%
Onset of action : 5–10
minutes
Peak response : 60–90 minutes
Duration of action : 4–10
hours
Plasma half-life : 2.5–4.5
hours
Primary route of metabolism: Hepatic;
active metabolite
Primary route of excretion: 50–60%
renal (unchanged)
Therapeutic serum concentration:
4–10 μg /mL
Clinical Uses
Procainamide is an effective
antiarrhythmic agent when given in sufficient doses at relatively short (3–4
hours) dosage intervals. Procainamide is
useful in the treatment of premature
atrial contractions, paroxysmal atrial tachy-cardia, and atrial fibrillation of
recent onset. Procainamide is
only moderately effective in converting atrial flutter or chronic atrial
fibrillation to sinus rhythm, although it has value in preventing recurrences of these
arrhythmias once they have been terminated by direct current (DC)
cardioversion.
Procainamide can decrease the
occurrence of all types of active ventricular dysrhythmias in patients with
acute myocardial infarction who are free from A-V dis-sociation, serious
ventricular failure, and cardiogenic shock. About 90% of patients with
ventricular prema-ture contractions and 80% of patients with ventricular
tachycardia respond to procainamide administration.
Although the spectrum of action
and electrophysio-logical effects of quinidine and procainamide are simi-lar,
the relatively short duration of action of pro-cainamide has tended to restrict
its use to patients who are intolerant of or unresponsive to quinidine.
Adverse Effects
Acute cardiovascular
reactions to procainamide admin-istration include hypotension, A-V block,
intraventricu-lar block, ventricular tachyarrhythmias, and complete heart
block. The drug dosage must be reduced or even stopped if severe depression of
conduction (severe pro-longation of the QRS interval) or repolarization (severe
prolongation of the QT interval) occurs.
Long-term drug use leads to
increased antinuclear antibody titers in more than 80% of patients; more than
30% of patients receiving long-term procainamide ther-apy develop a clinical
lupus erythematosus–like syn-drome. The symptoms may disappear within a few
days of cessation of procainamide therapy, although the tests for antinuclear
factor and lupus erythematosus cells may remain positive for several months.
Procainamide, unlike
procaine, has little potential to produce CNS toxicity. Rarely, patients may be
confused or have hallucinations.
Contraindications
Contraindications to
procainamide are similar to those for quinidine. Because of its effects on A-V
nodal and His-Purkinje conduction, procainamide should be ad-ministered with
caution to patients with second-degree A-V block and bundle branch block.
Procainamide should not be administered to patients who have shown procaine or
procainamide hypersensitivity and should be used with caution in patients with
bronchial asthma. Prolonged administration should be accompanied by
hematological studies, since agranulocytosis may occur.
Drug Interactions
The inherent anticholinergic
properties of procainamide may interfere with the therapeutic effect of
cholinergic agents. Patients receiving cimetidine and procainamide may exhibit
signs of procainamide toxicity, as cimetidine inhibits the metabolism of
procainamide. Simultaneous use of alcohol will increase the hepatic clearance
of pro-cainamide. Procainamide may enhance or prolong the neuromuscular
blocking activity of the aminoglycosides with the potential of producing
respiratory depression. The simultaneous administration of quinidine or
amio-darone may increase the plasma concentration of pro-cainamide.
Related Topics