Chapter: Clinical Anesthesiology: Anesthetic Management: Pediatric Anesthesia
Pediatric Anesthetic Techniques: Tracheal Intubation
Tracheal Intubation
One hundred percent oxygen should be adminis-tered prior to intubation
to increase patient safety during the obligatory period of apnea prior to and
during intubation. For awake intubations in neonates or infants, adequate
pre-oxygenation and continued oxygen insufflation dur-ing laryngoscopy (eg,
Oxyscope) may help prevent hypoxemia.
The infant’s prominent occiput tends to place
the head in a flexed position prior to intubation. This is easily corrected by
slightly elevating the shoulders with towels and placing the head on a
doughnut-shaped pillow. In older children, promi-nent tonsillar tissue can
obstruct visualization of the larynx. Straight laryngoscope blades aid
intuba-tion of the anterior larynx in neonates, infants, and young children
(Table 42–6). Endotracheal tubes that pass through the glottis may still
impinge upon the cricoid cartilage, which is the narrowest point of the airway
in children younger than 5 years of age. Mucosal trauma from trying to force a
tube through the cricoid cartilage can cause postoperative edema, stridor,
croup, and airway obstruction.
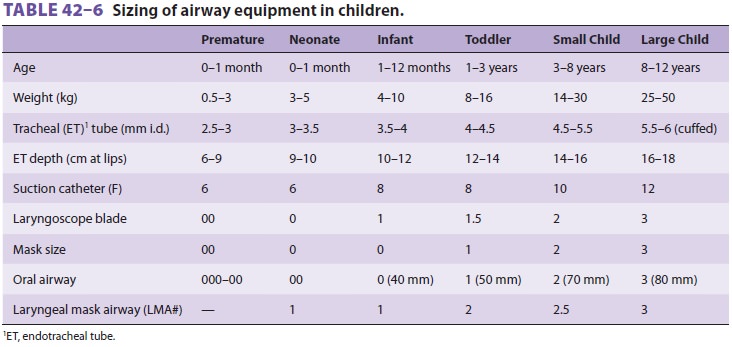
The appropriate diameter inside the endotra-cheal tube can be estimated
by a formula based on age:
4 + Age/4 = Tube diameter (in mm)
For example, a 4-year-old child would be
pre-dicted to require a 5-mm tube. This formula provides only a rough
guideline, however. Exceptions include premature neonates (2.5–3 mm tube) and
full-term neonates (3–3.5 mm tube). Alternatively, the practi-tioner can
remember that a newborn takes a 2.5- or 3-mm tube, and a 5-year-old takes a
5-mm tube. It should not be that difficult to identify which of the three sizes
of tube between 3 and 5 mm is required in small children. In larger children,
small (5–6 mm) cuffed tubes can be used either with or without the cuff
inflated to minimize the need for precise sizing. Endotracheal tubes 0.5 mm
larger and smaller than predicted should be readily available in or on the
anesthetic cart. Uncuffed endotracheal tubes tradi-tionally have been selected
for children aged 5 years or younger to decrease the risk of postintubation
croup, but many anesthesiologists no longer use size 4.0 or larger uncuffed
tubes. The leak test will mini-mize the likelihood that an excessively large
tube has been inserted. Correct tube size is confirmed by easy passage into the
larynx and the development of a gas leak at 15–20 cm H 2O pressure for an uncuffed tube. No leak
indicates an oversized tube that should be replaced to prevent postoperative
edema, whereas an excessive leak may preclude adequate ventilation and
contaminate the operating room with anesthetic gases. As noted above, many
clinicians use a down-sized cuffed tube with the cuff completely deflated in
younger patients at high risk for aspiration; minimal inflation of the cuff can
stop any air leak. There is also a formula to estimate endotracheal length:
12 + Age/2 = Length of tube (in cm)
Again, this formula provides only a guideline, and the result must be
confirmed by auscultation and clinical judgment. To avoid endobronchial
intu-bation, the tip of the endotracheal tube should pass only 1–2 cm beyond an
infant’s glottis. We favor an alternative approach: to intentionally place the
tip of the endotracheal tube into the right mainstem bron-chus and then
withdraw it until breath sounds are equal over both lung fields.
Related Topics