Chapter: Clinical Anesthesiology: Anesthetic Management: Pediatric Anesthesia
Pediatric Anesthetic Risk
PEDIATRIC ANESTHETIC RISK
The Pediatric Perioperative Cardiac Arrest
(POCA) Registry provides a useful database for assessing pediatric anesthetic
risk. This registry includes reports derived from approximately one million
pediatric anesthetics administered since 1994. Case records of children
experiencing cardiac arrests or death during the administration of or recovery
from anesthesia were investigated regarding any pos-sible relationship with
anesthesia. Nearly all patients received general anesthesia alone or combined
with regional anesthesia. In a preliminary analysis that included 289 cases of
cardiac arrest, anesthesia was judged to have contributed to 150 arrests. Thus
the risk of cardiac arrest in pediatric anesthetic cases would appear to be
approximately 1.4 in 10,000. Moreover, an overall mortality of 26% was reported
following cardiac arrest. Approximately 6% suffered permanent injury, but the
majority (68%) had either no or only temporary injury. Mortality was 4% in
American Society of Anesthesiologists (ASA) physi-cal status 1 and 2 patients
compared with 37% in ASA physical status 3–5 patients. It is important to note
that 33% of patients who suffered a cardiac arrest were ASA physical status
1–2. Infants accounted for 55% of all anesthesia-related arrests, with those
younger than 1 month of age (ie, neonates) having the greatest risk. As with
adults, two major predic-tors of mortality were ASA physical status 3–5 and
emergency surgery.
Most (82%) arrests occurred during induction of anesthesia; bradycardia,
hypotension, and a low Spo2 frequently preceded arrest.
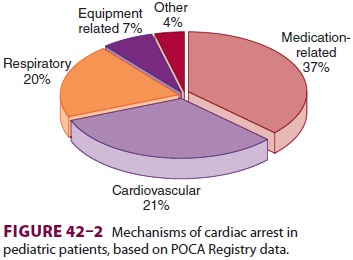
The most com-mon mechanism of cardiac arrest was judged to be medication
related (Figure 42–2). Cardiovascular depression
from halothane, alone or in combination with other drugs, was believed to be
responsible in
66% of all medication-related arrests. Another 9% was due to
intravascular injection of a local anes-thetic, most often following a negative
aspiration test during attempted caudal injection. Presumed cardiovascular
mechanisms most often had no clear etiology; in more than 50% of those cases
the patient had congenital heart disease. Where a cardiovascu-lar mechanism could
be identified, it was most often related to hemorrhage, transfusion, or
inadequate or inappropriate fluid therapy.
Respiratory mechanisms included laryngo-spasm, airway obstruction, and
difficult intubation (in decreasing order). In most cases the laryn-gospasm
occurred during induction. Nearly all patients who had airway obstruction or
were dif-ficult to intubate had at least one other significant underlying
disease.
The most common equipment-related mecha-nisms
that led to a cardiac arrest were complications related to attempted central
venous catheteriza-tion (eg, pneumothorax, hemothorax, or cardiac tamponade).
In recent years there has been increased
concern and scientific interest in the possibility that general anesthesia and
general anesthetic agents are toxic to the brains of small children. The
experimental data in animals are consistently worrisome, but the clinical data
are (currently) inconclusive as to the extent of the risk and whether one
technique is safer than another. Progress in this area can be followed on the
SmartTots web site (http://www.smarttots.org), maintained by the
International Anesthesia Research Society.
Children are at greater risk than adults of
devel-oping malignant hyperthermia.
Related Topics