Chapter: Clinical Anesthesiology: Anesthetic Management: Pediatric Anesthesia
Pediatric Anesthetic Techniques: Inhalational Induction
Inhalational Induction
Many children do not arrive in the operating room with an intravenous
line in place and nearly all dread the prospect of being stuck with a needle.
Fortunately, sevoflurane can render small children unconscious within minutes.
We find this easier in children who have been sedated (most often with oral
midazolam) prior to entering the operating room and who are sleepy enough to be
anesthetized without ever knowing what has happened (“steal” induction). One
can also insufflate the anesthetic gases over the face, place a drop of food
flavoring on the inside of the mask (eg, oil of orange), and allow the child to
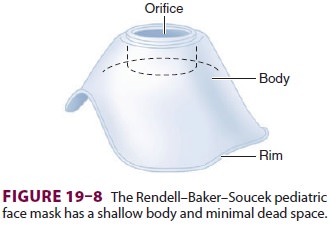
sit during the early stages of induction. Specially contoured masks minimize
dead space (see Figure 19–8).
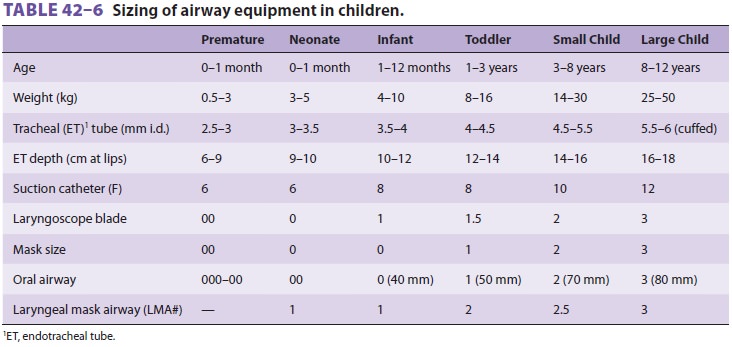
There are many differences between adult and
pediatric anatomy that influence mask ventilation and intubation. Equipment
appropriate for age and size should be selected (Table 42–6). Neonates and most young infants are obligate nasal breathers and
obstruct easily. Oral airways will help displace an oversized tongue; nasal
airways, so useful in adults, can traumatize small nares or prominent adenoids
in small children. Compression of submandibular soft tissues should be avoided
during mask ventila-tion to prevent upper airway obstruction.
Typically, the child can be coaxed into
breath-ing an odorless mixture of nitrous oxide (70%) and oxygen (30%).
Sevoflurane (or halothane) can be added to the gas mixture in 0.5% increments
every few breaths. As previously discussed, we favor sevo-flurane in most
situations. Desflurane and isoflu-rane are avoided for inhalation induction
because they are pungent and associated with more cough-ing, breath-holding,
and laryngospasm. We use a single (sometimes two) breath induction technique
with sevoflurane (7–8% sevoflurane in 60% nitrous oxide) to speed the
induction. After an adequate depth of anesthesia has been achieved, an
intrave-nous line can be started and propofol and an opi-oid (or a muscle
relaxant) administered to facilitate intubation. Patients typically pass
through an excite-ment stage during which any stimulation can induce
laryngospasm. Breath-holding must be distin-guished from laryngospasm.
Steady application of 10 cm of positive end-expiratory pressure will usu-ally
overcome laryngospasm.
Alternatively, the anesthesiologist can deepen the level of anesthesia
by increasing the concen-tration of volatile anesthetic, and place an LMA or
intubate the patient under “deep” sevoflurane anesthesia. Because of the
greater anesthetic depth required for tracheal intubation with the latter
tech-nique, the risk of cardiac depression, bradycardia, or laryngospasm
occurring without intravenous access detracts from this technique.
Intramuscular succinylcholine (4–6 mg/kg, not to exceed 150 mg) and atropine
(0.02 mg/kg, not to exceed 0.4 mg) should be available if laryngospasm or
bradycar-dia occurs before an intravenous line is established; intralingual
succinylcholine may be an alterative route (see above).
Positive-pressure ventilation during mask
induc-tion and prior to intubation sometimes causes gastric distention,
resulting in impairment of lung expansion. Suctioning with an orogastric or
nasogastric tube will decompress the stomach, but it must be done without
traumatizing fragile mucous membranes.
Related Topics