Chapter: Clinical Anesthesiology: Anesthetic Management: Pediatric Anesthesia
Pediatric Anesthetic Techniques: Maintenance
Maintenance
Ventilation is almost always controlled
during anesthesia of neonates and infants with a conven-tional semiclosed
circle system. During spontane-ous ventilation, even the low resistance of a
circle system can become a significant obstacle for a sick neonate to overcome.
Unidirectional valves, breath-ing tubes, and carbon dioxide absorbers account
for most of this resistance. For patients weighing less than 10 kg, some
anesthesiologists prefer the Mapleson D circuit or the Bain system because of
their low resistance and light weight. Nonetheless, because breathing-circuit
resistance is easily overcome by positive-pressure ventilation, the circle
system can be safely used in patients of all ages if ventilation is controlled.
Monitoring of airway pressure may provide early evidence of obstruction from a
kinked endotracheal tube or accidental advancement of the tube into a main-stem
bronchus.
Many anesthesia ventilators on older machines
are designed for adult patients and cannot reliably provide the reduced tidal
volumes and rapid rates required by neonates and infants. Unintentional
delivery of large tidal volumes to a small child can generate excessive peak
airway pressures and cause barotrauma. The pressure-limited mode, which is
found on nearly all newer anesthesia ventilators, should be used for neonates,
infants, and toddlers. Small tidal volumes can also be manually delivered with
greater ease with a 1-L breathing bag than with a 3-L adult bag. For children
less than 10 kg, ade-quate tidal volumes are achieved with peak inspira-tory
pressures of 15–18 cm H2O. For larger children the volume control ventilation may be used and
tidal volumes may be set at 6–8 mL/kg. Many spi-rometers are less accurate at
lower tidal volumes. In addition, the gas lost in long, compliant adult
breathing circuits becomes large relative to a child’s small tidal volume. For
this reason, pediatric tubing is usually shorter, lighter, and stiffer (less
compli-ant). Nevertheless, one should recall that the dead space contributed by
the tube and circle system consists only of the volume of the distal limb of
the Y-connector and that portion of the endotracheal tube that extends beyond
the airway. In other words, the dead space is unchanged by switching from adult
to pediatric tubing. Condenser humidifiers or heat and moisture exchangers
(HMEs) can add consider-able dead space; depending on the size of the patient,
they either should not be used or an appropriately sized, pediatric HME should
be employed.
Anesthesia can be maintained in pediatric
patients with the same agents as in adults. Some cli-nicians switch to
isoflurane following a sevoflurane induction in the hope of reducing the
likelihood of emergence agitation or postoperative delirium (see above). If
sevoflurane is continued for main-tenance, administration of an opioid (eg,
fentanyl, 1–1.5 mcg/kg) 15–20 min before the end of the procedure can reduce
the incidence of emergence delirium and agitation if the surgical procedure is
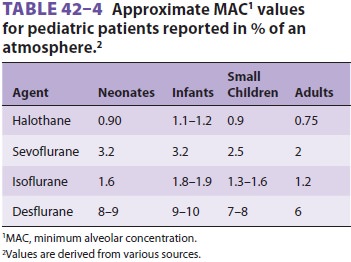
likely to produce postoperative pain. Although the MAC is greater in children
than in adults (see Table 42–4), neonates may be particularly sus-ceptible to
the cardiodepressant effects of general anesthetics. Neonates and sick children
may not tolerate increased concentrations of volatile agents required when the
volatile agent alone is used to maintain good surgical operating conditions.
Related Topics