Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Acid-Base Management
Metabolic Alkalosis
METABOLIC ALKALOSIS
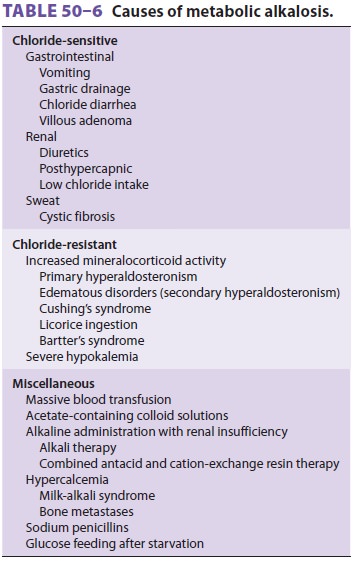
Metabolic alkalosis is defined as a primary increase in plasma [HCO3−]. Most cases of metabolic alka-losis
can be divided into (1) those associated with NaCl deficiency and extracellular
fluid depletion, often described as chloride sensitive, and (2) those
associated with enhanced mineralocorticoid activ-ity, commonly referred to as
chloride-resistant (Table 50–6).
Chloride-Sensitive Metabolic Alkalosis
Depletion of extracellular fluid causes the
renal tubules to avidly reabsorb Na+. Because not enough Cl− is available to accompany all of the Na+ ions reab-sorbed, increased H+ secretion must take place to maintain electroneutrality. In effect, HCO
3− ions that might otherwise have been excreted are reabsorbed, resulting
in metabolic alkalosis. Physiologically, maintenance of extracellular fluid
volume is there-fore given priority over acid–base balance. Because secretion
of K +
ion can also maintain electroneutral-ity, potassium secretion is also enhanced.
Moreover, hypokalemia augments H+ secretion (and HCO3− reabsorption) and will also propagate
metabolic alkalosis. Indeed, severe hypokalemia alone can cause alkalosis.
Urinary chloride concentrations during a chloride-sensitive metabolic alkalosis
are characteristically low (<10 mEq/L).
Diuretic therapy is the most common cause of chloride-sensitive metabolic alkalosis. Diuretics, such as furosemide, ethacrynic acid, and thiazides, increase Na+, Cl−, and K+ excretion, resulting in NaCl depletion, hypokalemia, and usually mild met-abolic alkalosis. Loss of gastric fluid is also a com-mon cause of chloride-sensitive metabolic alkalosis. Gastric secretions contain 25–100 mEq/L of H+, 40–160 mEq/L of Na+, about 15 mEq/L of K +, and about 200 mEq/L of Cl−. Vomiting or continu-ous loss of gastric fluid by gastric drainage(nasogastric suctioning) can result in marked meta-bolic alkalosis, extracellular volume depletion, and hypokalemia. Rapid normalization of Paco2 after plasma [HCO 3−] has risen in chronic respiratory aci-dosis results in metabolic alkalosis (posthypercapnic alkalosis; see above). Infants being fed formulas con-taining Na+ without chloride readily develop meta-bolic alkalosis because of the increased H+ (or K+) secretion that must accompany sodium absorption.
Chloride-Resistant Metabolic Alkalosis
Increased mineralocorticoid activity commonly results in metabolic
alkalosis, even when it is not associated with extracellular volume depletion.
Inappropriate increases in mineralocorticoid activ-ity cause sodium retention
and expansion of extra-cellular fluid volume. Increased H+ and K+ secretion takes place to balance enhanced mineralocorticoid-mediated
sodium reabsorption, resulting in meta-bolic alkalosis and hypokalemia. Urinary
chloride concentrations are typically greater than 20 mEq/L in such cases.
Other Causes of Metabolic Alkalosis
Metabolic alkalosis is rarely encountered in
patients given even large doses of NaHCO3 unless renal excretion of HCO 3− is impaired. The administra-tion of large
amounts of blood products and some plasma protein-containing colloid solution
fre-quently results in metabolic alkalosis. The citrate, lactate, and acetate
contained in these fluids are con-verted by the liver into HCO 3−.
Patients receiving high doses of sodium penicillin (particularly
car-benicillin) can develop metabolic alkalosis. Because penicillins act as
nonabsorbable anions in the renal tubules, increased H+ (or K+) secretion must accompany sodium absorption. For reasons that are not
clear, hypercalcemia that results from non-parathyroid causes (milk-alkali
syndrome and bone metastases) is also often associated with metabolic
alkalosis. The pathophysiology of alkalosis following refeeding is also
unknown.
Treatment of Metabolic Alkalosis
As with other acid–base disorders, correction
of metabolic alkalosis is never complete until the underlying disorder is
treated. When ventilation is controlled, any respiratory component
contribut-ing to alkalemia should be corrected by decreasing minute ventilation
to normalize Paco 2. The treat-ment of choice for chloride-sensitive metabolic alkalosis is
administration of intravenous saline (NaCl) and potassium (KCl). H 2-blocker therapy is useful when excessive
loss of gastric fluid is a fac-tor. Acetazolamide may also be useful in
edematous patients. Alkalosis associated with primary increase
in mineralocorticoid activity
readily responds to aldosterone antagonists (spironolactone). When arterial
blood pH is greater than 7.60, treatment with intravenous hydrochloric acid
(0.1 mol/L), ammo-nium chloride (0.1 mol/L), arginine hydrochloride, or
hemodialysis should be considered.
Related Topics