Chapter: Clinical Anesthesiology: Clinical Pharmacology: Pharmacological Principles
Isoflurane - Clinical Pharmacology of Inhalation Anesthetics
ISOFLURANE
Physical Properties
Isoflurane is a nonflammable volatile
anesthetic with a pungent ethereal odor. Although it is a chemical isomer with
the same molecular weight as enflurane, it has different physicochemical
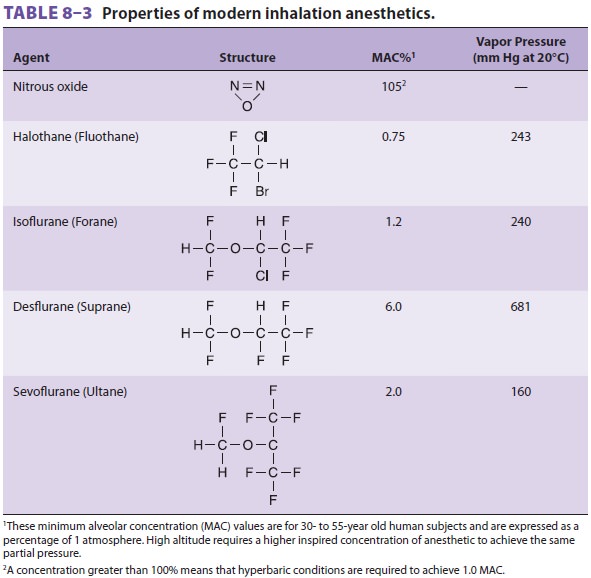
properties (see Table 8–3).
Effects on Organ Systems
A. Cardiovascular
Isoflurane causes minimal left
ventricular depression in vivo. Cardiac output is maintained by a rise in heart
rate due to partial preservation of carotid baro-reflexes. Mild β-adrenergic
stimulation increases skeletal muscle blood flow, decreases systemic vas-cular
resistance, and lowers arterial blood pressure. Rapid increases in isoflurane
concentration lead to transient increases in heart rate, arterial blood
pressure, and plasma levels of norepinephrine. Isofl urane dilates coronary arteries,
but not nearly as potently as nitroglycerin or adenosine. Dilation of normal
coronary arteries could theoreti-cally divert blood away from fixed stenotic
lesions, which was the basis for concern about coronary “steal” with this
agent, a concern that has largely been forgotten.
B. Respiratory
Respiratory depression during isoflurane
anesthesia resembles that of other volatile anesthetics, except that tachypnea
is less pronounced. The net effect is a more pronounced fall in minute
ventilation. Even low levels of isoflurane (0.1 MAC) blunt the normal
ventilatory response to hypoxia and hypercapnia.
Despite a tendency to irritate upper
airway reflexes, isoflurane is considered a good bronchodilator, but may not be
as potent a bronchodilator as halothane.
C. Cerebral
At concentrations greater than 1 MAC,
isoflurane increases CBF and intracranial pressure. These effects are thought
to be less pronounced than with halothane and are reversed by hyperventilation.
In contrast to halothane, the hyperventilation does not have to be instituted
prior to the use of isoflurane to prevent intracranial hypertension. Isoflurane
reduces cerebral metabolic oxygen requirements, and at 2 MAC, it produces an
electrically silent elec-troencephalogram (EEG).
D. Neuromuscular
Isoflurane relaxes skeletal muscle.
E. Renal
Isoflurane decreases renal blood flow,
glomerular fil-tration rate, and urinary output.
F. Hepatic
Total hepatic blood flow (hepatic artery
and portal vein flow) may be reduced during isoflurane anes-thesia. Hepatic
oxygen supply is better maintained with isoflurane than with halothane,
however, because hepatic artery perfusion is preserved. Liver function tests
are usually not affected.
Biotransformation & Toxicity
Isoflurane is metabolized to
trifluoroacetic acid. Although serum fluoride fluid levels may rise,
neph-rotoxicity is extremely unlikely, even in the presence of enzyme inducers.
Prolonged sedation (>24 h at 0.1–0.6% isoflurane) of critically ill
patients has resulted in elevated plasma fluoride levels (15–50 µmol/L) without
evidence of renal impairment. Similarly, up to 20 MAC-hours of isoflurane may
lead to fluoride levels exceeding 50 µmol/L without detectable postoperative
renal dysfunction. Its lim-ited oxidative metabolism also minimizes any
pos-sible risk of significant hepatic dysfunction.
Contraindications
Isoflurane presents no unique
contraindications. Patients with severe hypovolemia may not tolerateits
vasodilating effects. It can trigger malignant hyperthermia.
Drug Interactions
Epinephrine can be safely administered
in doses up to 4.5 mcg/kg. Nondepolarizing NMBAs are poten-tiated by
isoflurane.
Related Topics