Chapter: Clinical Anesthesiology: Clinical Pharmacology: Pharmacological Principles
Inhalation Anesthetics
Inhalation Anesthetics
Nitrous oxide, chloroform, and ether
were the first universally accepted general anesthetics. Methoxy-flurane and
enflurane, two potent halogenated agents, were used for many years in North
American anesthesia practice. Methoxyflurane was the most potent inhalation
agent, but its high solubility and low vapor pressure yielded longer inductions
and emergences. Up to 50% of it was metabolized by cytochrome P-450 (CYP)
enzymes to free fluoride (F−), oxalic acid, and other nephrotoxic
compounds. Prolonged anesthesia with methoxyflurane was as-sociated with a
vasopressin-resistant, high-output, renal failure that was most commonly seen
when F− levels increased to greater than 50
µmol/L. En-flurane has a nonpungent odor and is nonflammable at clinical
concentrations. It depresses myocardial contractility. It also increases the
secretion of ce-rebrospinal fluid (CSF) and the resistance to CSF outflow.
During deep anesthesia with hypocarbia electroencephalographic changes can
progress to a spike-and-wave pattern producing tonic–clonic sei-zures. Because
of these concerns, methoxyflurane and enflurane are no longer used.
Five inhalation agents continue to be
used in clinical anesthesiology: nitrous oxide, halothane, isoflurane,
desflurane, and sevoflurane.
The course of a general anesthetic can
be divid-ed into three phases: (1) induction, (2) maintenance, and (3)
emergence. Inhalation anesthetics, such as halothane and sevoflurane, are
particularly useful in the induction of pediatric patients in whom it may be
difficult to start an intravenous line. Although adults are usually induced
with intravenous agents, the nonpungency and rapid onset of sevoflurane make
inhalation induction practical for them as well. Regardless of the patient’s
age, anesthesia is often maintained with inhalation agents. Emergence depends
primarily upon redistribution from the brain and pulmonary elimination of these
agents.
Because of their unique route of
administration, inhalation anesthetics have useful pharmacological properties
not shared by other anesthetic agents. For instance, administration via the
pulmonary circula-tion allows a more rapid appearance of the drug in arterial
blood than intravenous administration.
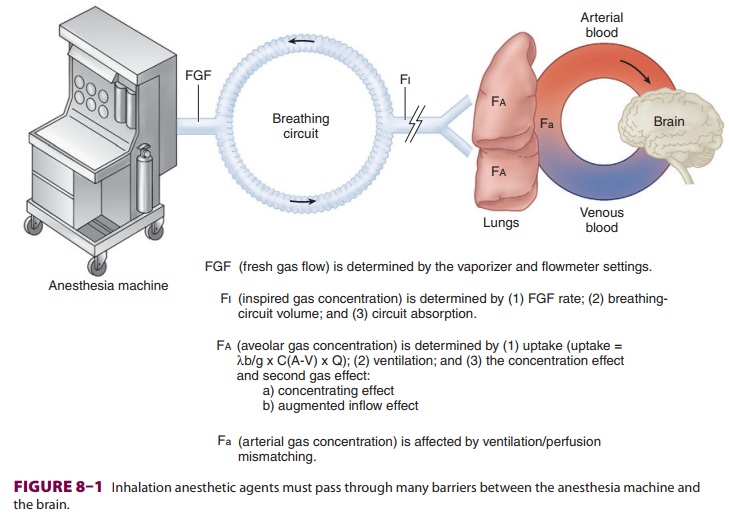
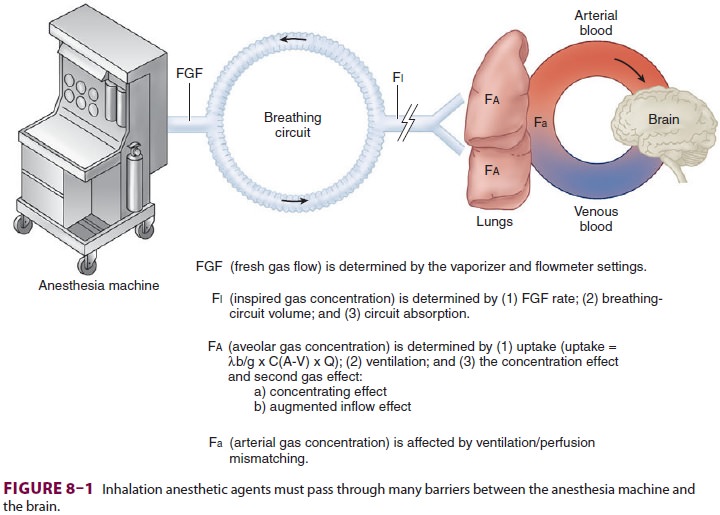
Pharmacokinetics of Inhalation Anesthetics
Although the mechanism of action of
inhalation anesthetics is complex, likely involving numerous membrane proteins
and ion channels, it is clear that producing their ultimate effect depends on
attainment of a therapeutic tissue concentration in the central nervous system
(CNS). There are many steps in between the anesthetic vaporizer and the
anesthetic’s deposition in the brain (Figure 8–1).
Related Topics