Chapter: 11th Zoology : Chapter 11 : Chemical Coordination and Integration
Human endocrine system
Human endocrine system
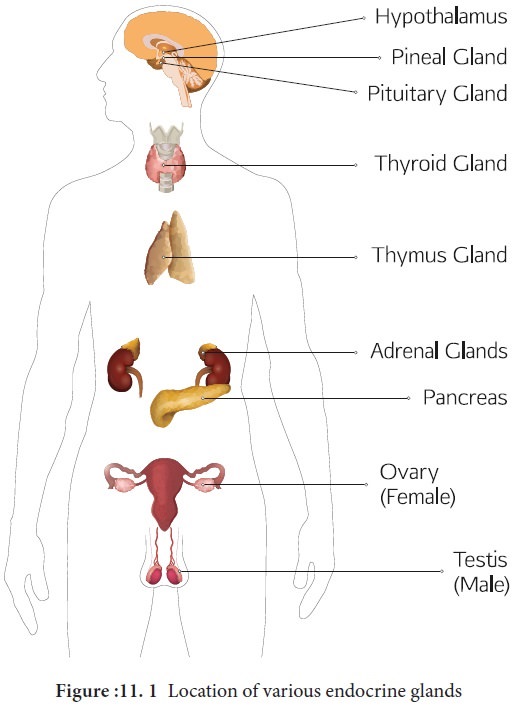
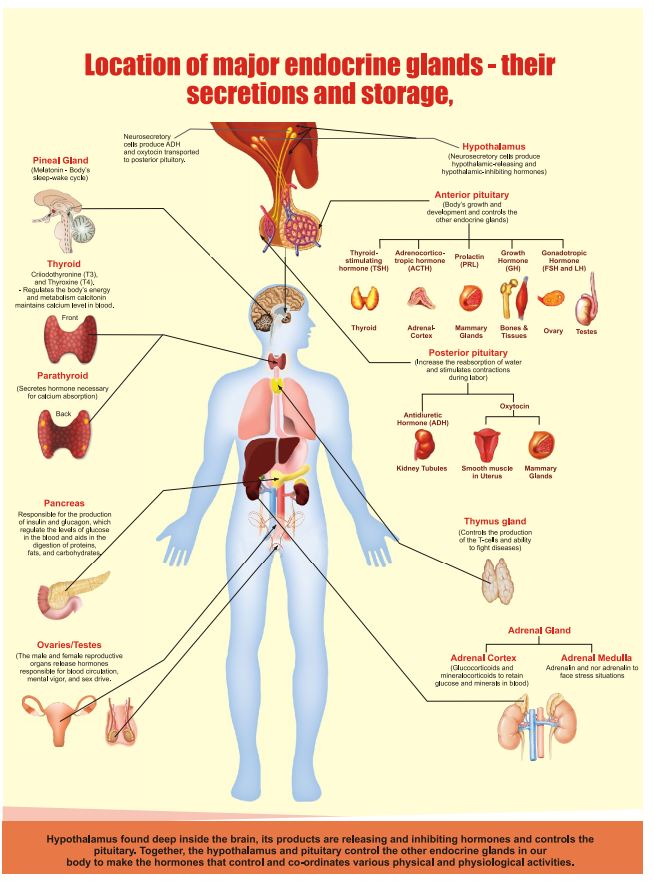
There are two glandular systems such as the
exocrine glands and the endocrine glands. The exocrine glands secrete enzymes,
saliva and sweat and have ducts that carry their substances to the membrane
surfaces. Example: salivary gland and gastric gland. The endocrine glands,
called ductless glands produce hormones and lack ducts; they release their
hormone to the surrounding tissue fluid. The hormones circulate around the body
and eventually reach the target organs. Endocrine glands (Figure: 11. 1)
include the pituitary, thyroid, parathyroid, pineal, adrenal, thymus and are
also known as exclusive endocrine glands. The hypothalamus along with its
neural function also produces hormones and is considered as a neuro endocrine
gland. In addition several organs such as pancreas, gastro intestinal tract
epithelium,kidney,heart, gonads and placenta are also have endocrine tissues
and are known as partial endocrine glands.
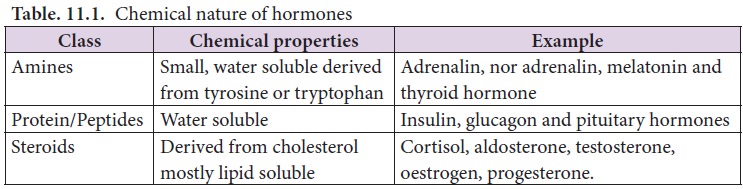
1. Hypothalamus
Hypothalamus is a small cone shaped structure that
projects downward from the brain ending into the pituitary stalk. It interlinks
both the nervous system and endocrine system. Though pituitary gland is known
as master endocrine glands that controls the other endocrineglands that
controls the other endocrine glands, but it is, in turn controlled by the
hypothalamus. Hypothalamus contains groups of neurosecretory cells.It produces
neurotransmitters which regulate the secretions of the pituitary
(Figure11. 2). The hormones produced by the hypothalamus act either as a
releasing hormone or as an inhibitory hormone.
In the basal region of the brain, the hypothalamic
hypophyseal portal blood vessel connects hypothalamus and anterior pituitary.
It allows hypothalamic hormones to control anterior pituitary secretion. The
posterior pituitary is connected with hypothalamus by a nerve bundle called
hypothalamic hypophyseal axis. It produces nerve signal that control the
posterior pituitary secretion. Hypothalamus maintains homeostasis, blood
pressure, body temperature, cardio and fluid electrolyte balance of the body.
As the part of limbic system it influences various emotional responses.
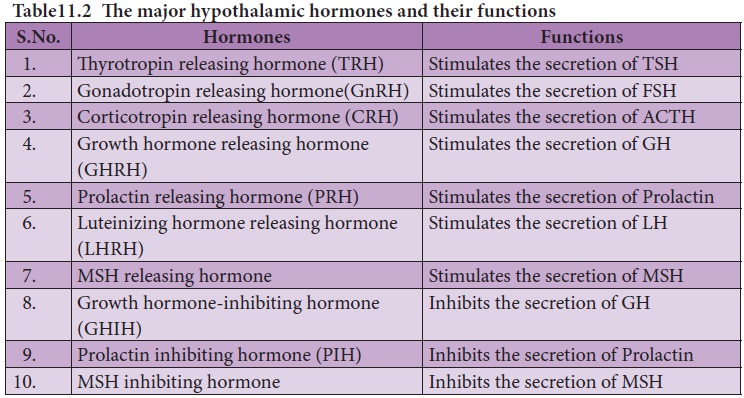
2. Pituitary gland or Hypophysis
The pituitary gland (means to grow under) is ovoid
in shape and is located in the sella
turcica, a bony cavity of the
sphenoid bone at the base of brain and connected to the hypothalamic region of the brain by a stalk called infundibulum. It is about one
centimetre in diameter and 0.5 gm in weight. The pituitary consists of two
lobes, anterior glandular adenohypophysis and posterior neural neurohypophysis.
The anterior lobe originates from the embryonic invagination of pharyngeal
epithelium called Rathke’s pouch and
the posterior lobe is originates from the base of the brain as an outgrowth of
hypothalamus. Anatomically the adenohypophysis has three lobes or zones namely
pars intermedia, pars distalis and pars tuberalis. The neurohypophysis is
otherwise known as pars nervosa.
The anterior lobe of pituitary secretes six tropic
hormones such as growth hormone (GH), thyroid stimulating hormone (TSH), adreno
corticotropic hormone (ACTH), follicle stimulating hormone (FSH),
luteinizing hormone (LH), luteotropic hormone (LTH) and melanocyte stimulating
hormone (MSH) (in lower animals only). The posterior lobe of pituitary secretes
the hormones namely vasopressin and oxytocin.
Hormones of Adenohypophysis
(i) Growth hormone (GH): It is also known as somatotropic hormone (STH) or Somatotropin. It is a peptide hormone. Growth hormone promotes growth of all the tissues and metabolic process of the body. It influences the metabolism of carbohydrates, proteins and lipids and increases the rate of protein biosynthesis in the cells. It stimulates chondrogenesis (cartilage formation), osteogenesis (bone formation) and helps in the retention of minerals like nitrogen, potassium, phosphorus, sodium etc., in the body. GH increases the release of fatty acid from adipose tissue and decreases the rate of glucose utilization for energy by the cells. Thus it conserves glucose for glucose dependent tissues, such as the brain.
ii)
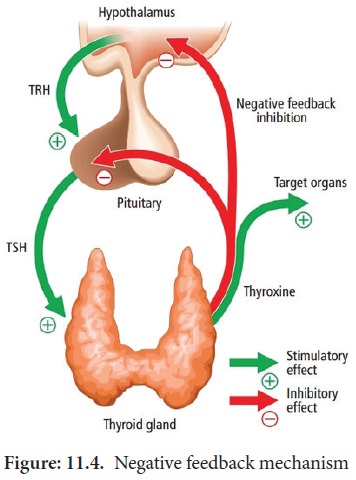
Thyroid
stimulating hormone (TSH) or thyrotropin: TSH is a glycoprotein hormone, which stimulates the thyroid gland to
secrete Tri-iodothyronine (T3) and thyroxine (T4). TSH secretion is regulated
by negative feedback mechanism.
It’s release from the anterior
pituitary is induced by the thyrotropin releasing hormone (TRH). When thyroxine
level in the blood increases, TRH acts on both the pituitary and hypothalamus
to inhibit TSH secretion.
(iii) Adreno
cortico tropic hormone (ACTH): ACTH is a peptide hormone that stimulates the adrenal cortex to
secrete glucocorticoids and mineralocorticoids. It stimulates melanin synthesis
in melanocytes, induces the release of fatty acids from adipose tissues and
stimulates insulin secretion. ACTH secretion is regulated by negative feedback mechanism.
(iv) Follicle
stimulating hormone (FSH): FSH is a glycoprotein hormone which regulates the functions of the gonads
(ovary and testis). In males, FSH along with androgens acts on the germinal
epithelium of seminiferous tubules and stimulates the production and release of
sperms (spermatogenesis). In females, FSH acts on the ovaries and brings about
the development and maturation of graffian follicles.
(v) Luteinizing
hormone (LH): LH is a glycoprotein hormone which is also known as interstitial cell stimulating hormone
(ICSH). In males, ICSH acts on the interstitial cells of testis to produce the
male sex hormone, testosterone. In females, LH along with FSH matures the
ovarian follicles. LH independently induces ovulation, maintains the corpus
luteum and promotes synthesis and release of ovarian hormones. FSH and LH are
collectively referred as gonadotropins. FSH and LH are not produced during
childhood. The secretion of FSH and LH starts only during pre pubertal period.
(vi) Luteotropic
hormone (LTH): LTH is also called luteotropin or lactogenic
hormone or prolactin or mammotropin.
It is a protein hormone which stimulates milk secretion after the child birth
in females. High prolactin secretion during lactation suppresses LH secretion
and ovulation since it induces the corpus luteum hence named as luteo tropic
hormone.
Hormones of neurohypophysis
i. Vasopressin
or antidiuretic hormone (ADH) : ADH is a peptide hormone which promotes reabsorption of water and
electrolytes by distal tubules of nephron and thereby reduces loss of water
through urine. Hence it is called as anti diuretic hormone. It also causes
constriction of blood vessels when released in large amount and increases blood
pressure. ADH deficiency causes Diabetes insipidus which induces the
production of large amount of urine.
ii. Oxytocin
(means
quick birth): It is a peptide hormone which stimulates vigorous contraction of the smooth muscles of
uterus during child birth and ejection of milk from the mammary glands.
3. Pineal gland
In human, the pineal gland or epiphysis cerebri or
conarium is located behind the third ventricle of brain and is formed of
parenchymal cells and interstitial cells. It secretes the hormone, melatonin, which plays a central role
in the regulation of circadian rhythm of our body and maintains the normal
sleep wake cycle. It also regulates the timing of sexual maturation of gonads.
In addition melatonin also influences metabolism, pigmentation, menstrual cycle
and defence mechanism of our body.
4. Thyroid gland
the butterfly shaped thyroid gland is a bilobed gland located below the larynx on each side of upper trachea. It is the largest endocrine gland in the body. Its two lateral lobes are connected by a median tissue mass called isthmus. Each lobe is made up of many lobules .The lobules consist of follicles called acini (acinus in singular). Each acinus is lined with glandular, cuboidal or squamous epithelial cells. The lumen of acinus is filled with colloid, a thick glycoprotein mixture consisting of thyroglobulin molecules.
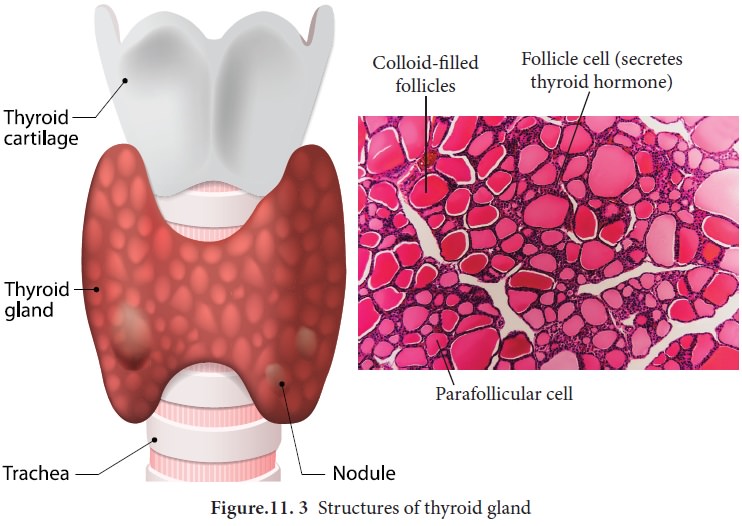
Hormones of the thyroid gland are often called the
major metabolic hormones. The follicular cells of thyroid gland secrete two
hormones namely tri-iodothyronine (T3 ) and thyroxine or tetra-
iodothyronine (T4). The parafollicular cells or ‘C’ cells of thyroid
gland secrete a hormone called thyrocalcitonin. Iodine is essential for the
normal synthesis of thyroid hormones. Thyroid releasing hormone from the
hypothalamus stimulates the adenohypophysis to secrete TSH, which inturn
stimulates the thyroid gland to secrete the thyroid hormones. Thyroid hormones
show a negative feedback effect on the hypothalamus and pituitary (Figure11.
4).
Functions
of thyroxine or tetra-iodothyronine (T4): Thyroxine regulates the basal metabolic rate (BMR) and body heat
production. It stimulates protein synthesis and promotes growth. It is
essential for the development of skeletal and nervous system. Thyroxine plays
an important role in maintaining blood pressure. It reduces serum cholesterol
levels, Optimum levels of thyroxine in blood is necessary for gonadial
functions.
Functions
of thyrocalcitonin (TCT): TCT is a polypeptide hormone, which regulates the blood calcium and phosphate
levels. It reduces the blood calcium level and opposes the effects of
parathyroid hormone.
5. Parathyroid gland
In human, four tiny parathyroid glands are found in
the posterior wall of the thyroid glands. This gland is composed of two types
of cells, the chief cells and oxyphil cells. The chief cells secrete
parathyroid hormone (PTH) and the functions of oxyphil cells are not known.
Parathyroid hormone or Parathormone (PTH)
PTH is a hypercalcemic
hormone. It is a peptide hormone involved in controlling the calcium and
phosphate homeostasis. The secretion of PTH is controlled by calcium level in
the blood. It increases the blood calcium level by stimulating osteoclasts to
dissolve the bone matrix. As a result calcium and phosphate are released into
the blood. PTH enhances the reabsorption of calcium and excretion of phosphates
by the renal tubules and promotes activation of vitamin D to increase calcium
absorption by intestinal mucosal cells.
6. Thymus gland
Thymus gland is partially an endocrine and
partially a lymphoid organ. It is a bilobed structure located just above the
heart and aorta, behind the sternum. It is covered by fibrous capsule and
anatomically it is
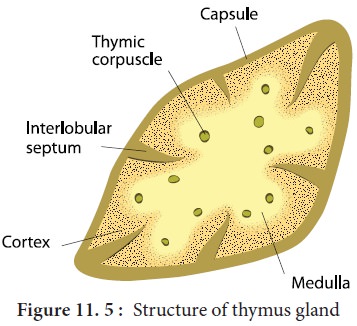
It secretes four hormones such as thymulin, thymosin, thymopoietin and thymic
humoral factor (THF). The primary function of thymus is
the production of immuno competent ‘T’ lymphocytes which provides cell mediated
immunity.
7. Adrenal gland
A pair of adrenal glands are located at the
anterior end of the kidneys, hence also called suprarenal glands. Anatomically
the outer region is the cortex and the inner region is the medulla.
Histologically the adrenalcortexhasthreedistinctzones,zona glomerulosa, zona
fasciculata and zona reticularis. Zona
glomerulosa an outer thin layer constitutes about 15% of adrenal cortex,
and secretes mineralocorticoids. Zona
fasciculata, the middle widest layer
constitutes about 75% of adrenal cortex and
secretes glucocorticoids such as cortisol, corticosterone and trace amounts
of adrenal androgen and oestrogen. Zona
reticularis, an inner zone of adrenal cortex constitute about 10% of
adrenal cortex and secretes the adrenal androgen, trace amount of oestrogen and
glucocorticoids.
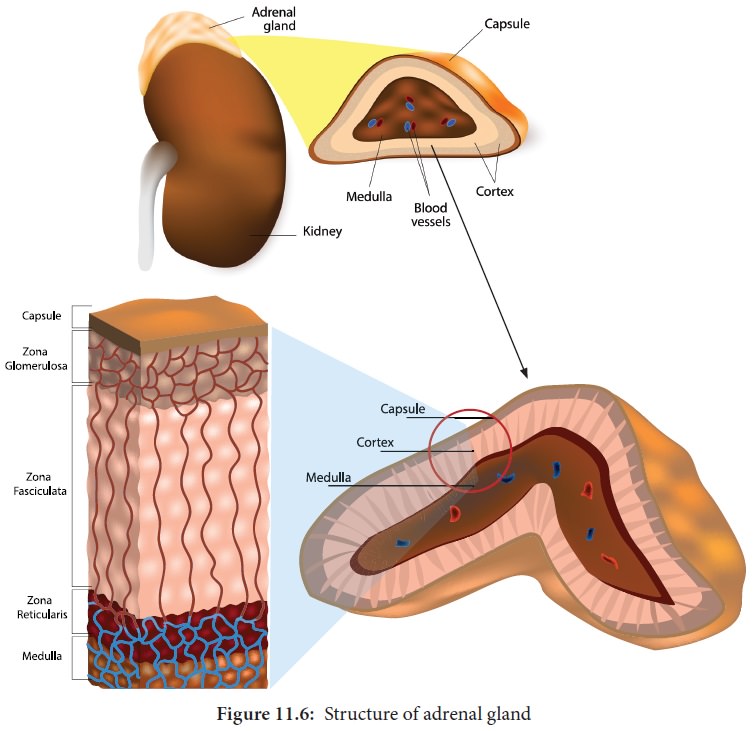
Adrenal medulla: It is the central part of adrenal gland and is composed of ovoid and columnar cells, which are found around the network of blood capillaries. Adrenalin (epinephrine) and nor adrenalin (nor epinephrine) are the two hormones secreted by the adrenal medulla. Both adrenalin and nor adrenalin are catecholamines.
Function
of adrenal hormones:
Glucocorticoids stimulate gluconeogensis, lipolysis and proteolysis (the life saving activity). Cortisol is a glucocorticoid involved in maintaining cardio
vascular and kidney functions. It produces anti-inflammatory reactions and
suppresses the immune response. It stimulates the RBC production. It is also
known as stress combat hormone. Mineralocorticoids
regulates water and electrolyte balance of our body. Aldosterone stimulates the reabsorption of sodium and water and
eliminates potassium and phosphate ions through excretion, thus it helps in
maintaining electrolytes, osmotic pressure and blood pressure. Adrenal androgen
plays a role in hair growth in the axial region, pubis and face during puberty.
The adrenal
medulla secretes the hormones adrenalin and noradrenalin and are referred
as "3F hormone" (fight, flight and fright hormone). Adrenalin
increases liver glycogen breakdown into glucose and increases the release of
fatty acids from fat cells. During emergency it increases heart beat rate and
blood pressure. It stimulates the smooth muscles of cutaneous and visceral
arteries to decrease blood flow. It increases blood flow to the skeletal
muscles thereby increases the metabolic rate of skeletal muscles, cardiac
muscles and nervous tissue.
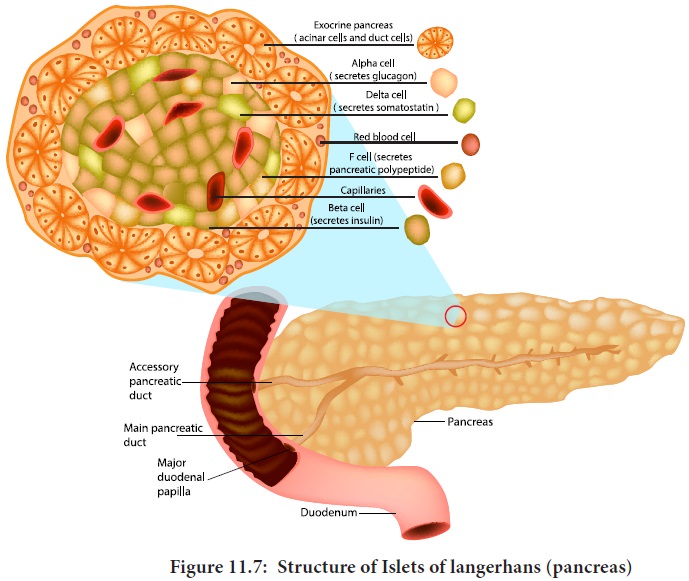
8. Pancreas
Pancreas is a composite gland which performs both
exocrine and endocrine functions.
It is located just below the stomach as a leaf like
structure. The pancreas is composed of two major tissues such the acini and
islets of langerhans. Acini secretes digestive enzymes and the islets of
langerhans secretes hormones like insulin and glucagon.
Human pancreas has one to two million islets of
langerhans. In each islet about 60% cells are beta cells, 25% cells are alpha
cells and 10% cells are delta cells. The alpha cells secrete glucagon, the beta
cells secrete insulin and delta cells secrete somatostatin.
Insulin: Insulin
is a peptide hormone and plays an important role in glucose homeostasis. It’s main effect is to lower blood glucose levels by
increasing the uptake of glucose into the body cells,
especially muscle and fat cells. Insulin also inhibits the breakdown of
glycogen to glucose, the conversion of amino acids or fats to glucose, so
insulin is rightly called a hypoglycemic hormone.
Glucagon:
Glucagon
is a polypeptide hormone. It is a potent hyperglycaemic hormone that acts on the liver and promotes the breakdown of
glycogen to glucose (Glygogenolysis), synthesis of glucose from lactic acid and
from non-carbohydrate molecules (Gluconeogenesis) . Glucagon releases glucose
from the liver cells, increasing the blood glucose levels. Since glucagon
reduces the cellular uptake and utilisation of glucose it is called a
hyperglycemic hormone. Prolonged hyperglycemia leads to the disorder called
diabetes mellitus.
9. Gonads
Testis: A pair of
testis is present in the scrotal sac of males. The testis functions as a sex organ and also as an endocrine
gland. The testis is composed of seminiferous tubules and interstitial cells or
Leydig cells. The Leydig cells secrete several male sex hormones, collectively
called androgens, mainly testosterone.
Functions
of testosterone: Under the influence of FSH and LH, testosterone
initiates maturation of male
reproductive organs, and the appearance of secondary sexual characters,
muscular growth, growth of facial and axillary hair, masculine voice and male
sexual behaviour. It enhances the total bone matrix and plays a stimulating
role in the process of spermatogenesis.
Ovary: Females
have a pair of ovaries located in the pelvic region of
The ovary is composed of ovarian
follicles and stromal tissues. It produces the eggs or ova. The ovaries secrete
the steroid hormones oestrogen and progesterone. Oestrogen is responsible for the maturation of reproductive organs
and the development of secondary sexual characters at puberty. Along with
progesterone, oestrogens promotes breast development and initiate the cyclic
changes during menstrual cycle. Progesterone
prepares the uterus for implantation of the fertilized ovum. It
decreases the uterine contraction during pregnancy and stimulates the
development of mammary glands and milk secretion. It is responsible for
premenstrual changes in the uterus and is essential for the formation of
placenta.
10. Hormones of heart, kidney and gastro intestinal tract
Some tissues of the heart, kidney and gastro
intestinal tract acts as partial endocrine glands. In the heart, cardiocytes on
the atrial wall's secretes an important peptide hormone called atrial
natriuretic factor (ANF). When blood pressure is increased, ANF is secreted and
causes dilation of the blood vessels to reduce the blood pressure.
In kidneys, hormones such as renin, erythropoietin
and calcitriol are secreted.
Renin is
secreted by juxta glomerular cells (JGA), which increases blood pressure when angiotensin is formed in blood. Erythropoietin is also secreted by the
JGA cells of the kidney and stimulates erythropoiesis (formation of RBC) in
bone marrow. Calcitriol is sercreted
by proximal tubules of nephron. It is an active form of vitamin D3 which promotes calcium and
phosphorus absorption from intestine and accelerates bone formation.
Gastro intestinal tract hormones
Group of specialized endocrine cells present in
gastro-intestinal tract secretes hormones such as gastrin, cholecystokinin
(CCK), secretin and gastric inhibitory peptides (GIP). Gastrin acts on the gastric glands and stimulates the secretion of
HCl and pepsinogen. Cholecystokinin
(CCK) is secreted by duodenum in response to the presence of fat and acid
in the diet. It acts on the gall bladder to release bile into duodenum and
stimulates the secretion of pancreatic enzymes and its discharge. Secretin acts on acini cells of
pancreas to secrete bicarbonate ions and water to neutralize the acidity. Gastric
inhibitory peptide (GIP) inhibits gastric secretion and motility.
Related Topics