Chapter: Medicine Study Notes : Gastro-Intestinal
Hepatitis B - Liver Disease
Hepatitis B
Epidemiology
·
350 million with chronic
infection, >75% of these Asian
·
30% of chronically infected die
prematurely from the disease
·
In NZ, approx. 50,000
carriers. Chinese 10%, Maori 5.4%, PI
4.4%, European 0.43%
·
Transmission:
o Body fluids (blood, semen), including transfusion & contaminated needles
o Mother to baby (vertical transmission): 95% risk of infection –
vaccinate at birth and give Anti-HBs – immune globulin
o Organ transplant
o Child to child (horizontal transmission). Must get into blood – e.g.
grazes, stubbed toes. Very resilient virus. Children are most likely to have
asymptomatic seroconversion
Diagnosis
·
ALT elevation to 1000-1500
(usually higher than for Hep C)
·
Viral antigens:
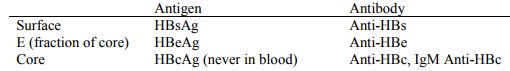
·
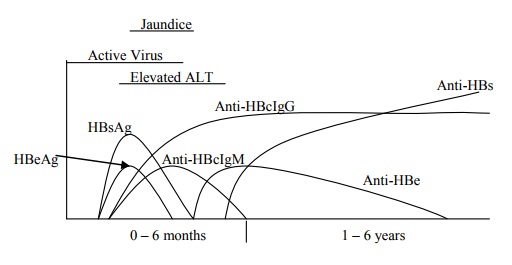
Acute Viral Hepatitis due to HBV
with recovery:
·
Jaundice
·
Diagnosis from bloods:
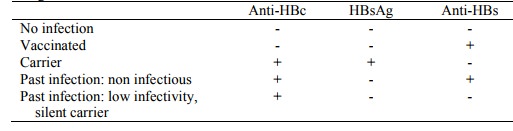
o With HBsAg, HBeAg, and HBV DNA by PCR.
o Acute HBV: IgM Anti-HBc
o Carrier: HBsAg
o Past infection: IgG Anti-HBc
o Vaccine immunity: IgG Anti-HBs > 10 IU
·
Monitoring for carrier state:
Test for HBsAg:
o Monthly for first 6 months or until negative
o If still positive at 6 months then probably carrier: test 6 monthly till
2 years
o Annually thereafter
o Also test ALT
·
Carrier infectivity:
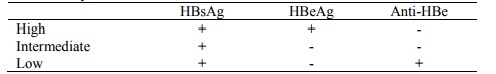
o Presence of HBe has a high correlation with the presence of whole
hepatitis virons in the blood
·
Screening:
·
Normal virus called „wild type‟.
Also pre-core mutant HBV virus – doesn‟t produce E antigen but will still be
HBV-DNA +ive
Progression
·
Incubation 45 – 180 days
·
Symptoms:
o Incubation: can be up to 6 months or longer
o Minority of first episodes are symptomatic
o If symptoms occur: malaise, anorexia, nausea, jaundice. Coincide with
appearance of Anti-HBc antibody in serum
·
Acute HBV infection leads to:
o 10% chronic infection („carrier‟ is a misnomer) due to ineffective immune response. 90% of infected newborn infants, 25% in young children, and 2 % adults. 25% of „carriers‟ develop chronic active hepatitis and cirrhosis, and 50% have hepatocellular carcinoma peaking in the 5th decade
o 65% transient subclinical infection ® 100% recovery
·
25% acute hepatitis ® 99%
recover, 1% ® fulminant hepatitis
·
Stages of illness:
o Immune tolerant stage (mainly babies): no hepatitis even though circulating virus. HBsAg, HbeAg in blood
o Immune activation ® ALT
o If chronic: called chronic lobular hepatitis (CLH) or chronic active hepatitis (CAH). 6% will clear it per year. Key issue is how much fibrosis has occurred before clearance
o First stage of clearance: E antigen seroconvesion. ¯HBeAg and anti-HBe (was there previousl – but used up too rapidly to detect. As HBeAg¯, residual anti-HBe)
o Second stage: S antigen seroconversion
Vaccination
·
Most effective means of control:
vaccination: Engerix B. 85 – 90%
efficacy
·
Yeast derived subunit vaccine.
·
Number of notifications has
dropped from 400 to 100 since introduction in 1988
· Suspension of synthetic HBsAg
·
Doses at 0, 1 and 6 months ® immune
levels of Anti-HBs in 92%.
·
Check for seroconversion 2 months
later
·
Booster every 2 – 3 years if high
risk
Treatment
·
Lamivudine
o Purine nucleoside analogue: inhibits DNA polymerase. Potent inhibitor of HBV replications
o As safe as placebo, no interactions, excreted unchanged
·
Each year of treatment:
o 17% HBe seroconversion (30% if concurrent interferon)
o 15% get YMDD mutant ® ALT and HBV DNA again. But these also seem to seroconvert in time
o Eligibility:
§ If ALT > 2 * normal
§ Pre & post liver transplant
§ HIV and HBV co-infection (plus multi drug therapy for HIV as well)
·
Risk of Hepatocellular carcinoma
– related to length of time as a carrier
Related Topics