Chapter: Medicine Study Notes : Gastro-Intestinal
Assessment - Liver Disease
Liver Disease
·
NB: This section combines notes
from the Gut run, and from Microbiology and Chemical Pathology
Assessment
Presentation
·
Found coincidentally when
clinically well (e.g. medicals)
· Family screening e.g. abnormal irons, HBV
·
Non-specific illness and found to
have abnormal LFT: ?alcohol, medicines, viral, jaundice, liver/bilary disease
·
Is it acute, chronic, acute on
chronic, or a failing chronic
Aetiology
·
Acute hepatitis:
o Viral: A, B, C, D, others
o Toxic:
§ Drugs
§ Poisoning (eg alcohol)
·
Chronic hepatitis:
o Viral: B, C, B + D, CMV
o Toxic:
§ Drugs
§ Chronic Alcohol
o Autoimmune
o Metabolic:
§ Alpha-1-antitrypsin
o Wilson‟s disease
o Haemochromatosis
·
Fatty liver: Obesity, NIDDM,
Drugs, alcohol
History
·
Surgery: e.g. cholecystectomy
·
Heart disease: congestive heart
failure
·
Pregnancy
·
HIV positive, sexual orientation
·
Contact with hepatitis: family,
sexual
·
Travel: malaria, parasites
· Hepatitis infection risk: Tattoos, body piercing, health care worker, transfusion, IVDU
·
Alcohol ® acute
alcoholic hepatitis
·
Ethnic group
· Medications – ALWAYS ASK ABOUT DRUGS
· Family History: e.g. anaemias, Gilbert‟s syndrome, haemochromatosis, gallstones, alcoholism, autoimmune disease, Wilson‟s disease (copper)
·
Symptoms: itch, urine and stool
colour
Liver Function Tests (LFTs)
·
Investigations:
o Bloods:
§ Bilirubin
§ LFT: AST, ALT, ALP, GGT
§ Total protein, albumin
§ Tests can be widely variable for the same condition
§ Other: Coagulation studies, ammonia
§ Special tests: a1 antitrypsin, afeta protein, hepatitis markers, specific autoantibodies, Igs, caeruloplasmin
§ Any liver disorder may ® Âferritin (also an acute phase protein)
o Also test for other causes of liver disease: HBV, HIV, iron studies (ferritin), immune liver disease (ÂAnti-nuclear Antibodies – ANA)
o Imaging: ultrasound +/- CT, MRCP, ERCP. Ultrasound and CT have high
false negatives for bilary
o Percutaneous transhepatic cholangiogram – PCT
o Liver biopsy the gold standard
· Aim to decide if liver disease is present, is progressing or is severe
·
Aiming to answer three questions:
·
Is there liver cell death –
inflammation and hepatonecrosis? Check:
o Bilirubin: in acute hepatitis will be 50:50 direct and indirect
o Raised aminotransferases predominate. If AST > ALT think severe
cirrhosis, liver malignancy, alcohol. In normal hepatitis ALT > AST
o Common liver causes:
§ Non-alcoholic steatohepatitis (fatty liver): probably the most common
cause of mildly elevated LFTs, especially if obese, Type 2 diabetes and
hyperlipideamia
§ Acute/chronic viral hepatitis
§ Genetic haemochromatosis
§ Autoimmune hepatitis
§ Less commonly: a1 antitrypsin deficiency and Wilson‟s disease
o Causes of abnormal LFTs other than Liver disease:
§ Diseases of other organs affecting liver, e.g. RA
§ Medicines, alcohol, tonics, remedies, poisons
§ Congestive heart failure ® hepatic congestion
o AST: also produced by:
§ Muscle: If normal ALT and ÂAST then
do a CK for muscle breakdown
§ Blood: Haemolysis
·
Is there cholestasis (=impaired
bile flow)? Liver can remove 5 * normal bilirubin from circulation (i.e. large
functional reserve). Cholestasis usually refers to obstruction within the
liver. „Obstructive Jaundice‟ Þ major ducts. Bile salts are 90% reabsorbed in the terminal ileum. They
emulsify fats. Bile also contains cholesterol, phospholipids and bilirubin
(reabsorbed ® urobilinogen ® urine)
o If left or right hepatic duct blocked, other side of liver will
be sufficient to keep bilirubin normal
o GGT released in inflammation: usually in parallel with ALP in
obstruction. If ÂGGT and ÂALP then ALP is from the bilary tree
o Raised ALP and GGT predominate in cholestatic diseases
o Common:
§ Biliary obstruction: gallstones
§ Drug hepatotoxicity
§ Neoplasms (eg head of pancreas)
o Less Common:
§ Primary biliary cirrhosis
§ Primary sclerosing cholangitis
§ Sarcoidosis
§ Autoimmune cholangiopathy
o Other causes of ÂALP:
§ ALP from bone and cholangiocytes (bilary epithelium). Excreted in urine,
but saturated kinetics ® Âserum level
§ Physiological:
·
Bone: Growth and fractures. High in puberty
·
Pregnancy (placental)
·
Benign  with age
§ Bone disease: Paget‟s, malignancy, renal failure, hyperparathyroidism,
Rickets
§ GI tract can also produce ALP, eg Crohn‟s
§ Miscellaneous: hyperthyroidism, familial benign, transient of infancy
o GGT Â benignly with age and obesity
·
Is liver function normal? Are
detoxification, synthesis, and glucose management working? Has a large
functional reserve. Check:
o Bilirubin
o Albumin. See below
o Prothrombin time (INR): factors 2, 5, 7, 9, 10. Give parental Vitamin K
to differentiate between malabsorption or poor liver function
·
Tests in cirrhosis
o Liver function tests very variable:
§ Quiescent phase: normal of minor  in LFT
§ Active Phase:  in ALT and AST when necrosis is dominant
o Causes: idiopathic, alcohol, chronic active hepatitis, primary biliary
cirrhosis, haemochromatosis, Wilson‟s disease, a1
antitrypsin deficiency
·
Other examples of Liver Function
tests:
o ÂÂALT and ÂÂAST: viral hepatitis, Paracetamol OD
o ÂALP and Âbilirubin in a 12 year old with vomiting: Gilbert‟s syndrome (Âbilirubin when fasting), ALP normally raised at this age
o ÂBilirubin,
ÂALP, ÂŻAlbumin + neuro signs ® ?Wilson‟s disease (very rare)
o ÂBilirubin,
ÂALP, ÂŻAlbumin + abnormal electrophoresis ® ? ÂŻa1
antitrypsin
Total Protein
·
Normal Ranges:
Albumin 34 – 46
Globulin Gap ~ 20
·
Examples:
o 55 year old man, ÂŻalbumin, normal protein Ăž ÂIg (common in cirrhosis)
o 14 year old, Âcholesterol, ÂŻprotein, ÂŻalbumin Ăž nephrotic syndrome (relevance of high cholesterol not understood)
o 58 year old man with diabetes, protein 94, albumin 56 Ăž
dehydration (don‟t get albumin > 50 without dehydration)
o 40year old post-op, protein 26, albumin 11 Ăž
dilution. Took blood downstream of iv
line
o 46 year old, enlarged nodes, protein 50, albumin 33 Ăž ÂŻ globulin
gap Ăž ? immunocompromised/lymphoma
o 60 year old, pneumonia, protein 70, albumin 22 Ăž acute
phase + maybe ÂIg
o 50 year old, recurrent abdominal pain, protein 55, albumin 27 Ăž
pancreatitis ® malabsorption
o 38 year old, SOB, rash, protein 86, albumin 34 Ăž
sarcoidosis or SLE
·
Differentials:
o Hypoproteinaemia:
§ Haemodilution: poor iv therapy, drip arm, SIADH, pregnancy
§ ¯Albumin: ¯synthesis
(liver disease, malabsorption, malnutrition), losses (renal, gut, skin),
non-specific (eg illness)
§ ¯Ig:
primary or secondary immunodeficiencies. Only IgG deficiency is enough to show
up as low protein or on electrophoresis
o Hyperproteinaemia:
§ Haemoconcentration: dehydration, haemostasis
§ ÂIg:
·
Monoclonal: myeloma, lymphoma,
macroglobulin, MGUS
·
Polyclonal: liver disease,
infection, autoimmune, sarcoidosis
·
Oligoclonal
Aside: Electrophoresis
·
Bands: albumin, a1
antitrypsin, haptaglobins (a2 band), transferrin, complement, Igs
·
Two indications:
o a1
antitrypsin deficiency
o Monoclonal antibody band
· Monoclonal Gammaglobulinaemia of Uncertain Significance (MGUS)
o Benign, but potential for malignant transformation (eg to Myeloma): 5% at 5 years, 25% at 15 years
o Ăž need to
follow up over time
o See Aside: Conditions associated with Monoclonal proteins
Causes of Jaundice
· For neonatal jaundice
·
Unconjugated hyperbilirubinaemia
o Overproduction: Intravascular or extrahepatic haemolysis
o ÂŻ Hepatocellular uptake: drugs, sepsis, starvation
o ÂŻ
Hepatocellular conjugation: Gilbert‟s syndrome, neonatal jaundice, drugs,
diffuse hepatic disease
·
Conjugated bilirubinaema
(cholestatic jaundice)
o Impaired hepatocellular secretion: various syndromes, duct stricture, biliary cirrhosis, steroids
o Hepatocellular cholestasis – impaired secretion plus liver injury as
well: viral infection, drugs, alcohol
o Extrahepatic obstruction: stones, carcinoma, strictures and congenital
atresia
Pathology
·
Normal histology:
o Chords of hepatocytes between sinuses running from portal tract to
central vein
o Zone 3 (perivenular) more sensitive (eg to drugs) than zone 1
(periportal)
·
Acute Hepatitis:
o =Inflammation of the liver: no cause implied
o Macroscopic appearance: mildly enlarged, tender liver. Flu like symptoms. Jaundice, itching
o Microscopic appearance:
§ Diffuse liver cell injury with lobular disarray: loss of normal radial array
§ Focal necrosis of hepatocytes with hepatocyte regeneration (mitotic figures, variation in cell size)
§ Portal inflammation: lymphocytes & macrophages. Eosinophils with drugs
§ Bile stasis: variable (often absent), due to disruption of canaliculi,
greenish
§ NO fibrosis
·
Chronic hepatitis:
o If longer than 6 months then chronic – otherwise acute (unless chronic
signs – e.g. spider naevi)
o Chronic active and chronic persistent hepatitis reflect different
disease activity but caused by the same agents
o Chronic persistent hepatitis: Benign and self-limiting, following acute
hepatitis and lasting several years. Inflammation limited to portal triad
(lymphocytes, macrophages and plasma cells). Architecture preserved, no
fibrosis, no hepatocyte necrosis
o Chronic active hepatitis:
§ Progressive hepatic necrosis and fibrosis, potentially leading to
cirrhosis
§ Clinical course variable. 5 year
survival 25 – 50%
§ Marked portal inflammation extending into lobules
§ Piecemeal necrosis: „nibbling away‟ at hepatocytes around portal track
by lymphocytes ® necrosis
§ Bridging necrosis: creating portal-central or portal-portal tracts
§ Hepatitis B: ground glass hepatocytes – large, uniform cytoplasm filled
with viral protein
§ Hepatitis C: fatty degeneration, bile duct lesions and lymphoid
follicles
·
Fulminant Hepatitis:
o Very rare. Onset to death in 2 – 3 weeks (massive necrosis) to 3 months (submassive failure)
o Causes: Viral (60%), drugs/chemicals (30%, eg paracetamol poisoning),
numerous other minor causes
o Macroscopic appearance: all/most of liver destroyed. Red, limp, wrinkled capsule. Mushy red
o Microscopic appearance: Zonal (2,3) or complete necrosis, liquefaction
of hepatocytes, little inflammation
Management of Acute Hepatitis
·
Avoid strenuous physical activity
while jaundiced, increase slowly afterwards
·
Best rest only if unwell
·
No corticosteroids
·
Perhaps reduce fat, abstinence from
alcohol
·
Care with personal hygiene
·
Follow liver tests until normal
Progression of Chronic Hepatitis
·
Acute hepatitis
(inflammation/cell death) ® regeneration ® resolution or chronic
hepatitis, which may ® fibrosis (the necessary step for progression to liver failure) ®
disordered architecture ® cirrhosis
·
Assessing Liver Biopsy:
o Is there inflammation around the portal tract? „Limiting plate‟ surrounds portal tract. Monocytes migrate through this and cause piecemeal or interface hepatitis. If it extends to another portal tract then called bridging necrosis
o Is there inflammation/necrosis out in the lobule Ăž
intralobular or focal necrosis
o Are there inflammatory cells in the portal tract Ăž portal
inflammation
o How much scar tissue/fibrosis is there?
o Knodell index scores each of these to generate a Hepatitis Activity
Index (HAI). Score out of 22
·
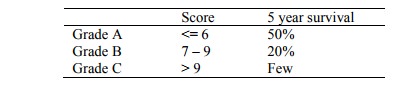
Child-Pugh Classification of
liver function/failure: sum of scores for encephalopathy, ascites, bilirubin,
albumin, INR, nutrition
Related Topics