Chapter: Biology of Disease: Diet and Disease
General Management of Nutritional Disorders
GENERAL MANAGEMENT OF NUTRITIONAL
DISORDERS
Patients who are malnourished or at risk of developing
malnutrition require appropriate therapy, which ranges from simple dietary advice
to long-term parenteral nutrition. The dietary needs of the patient must be
carefully assessed to provide the correct amounts of energy, protein, vitamins,
minerals and trace elements. Patients receive these diets by oral (Figure 10.39), tube and parenteral
feeding; the last is most commonly administered by intravenous infusion. Oral
supplementation should be used wherever possible and the common practice is to
encourage consumption of specific foods or supplements that rectify the
nutritional disorder in question. In cases where oral feeding is not possible,
then liquid food is administered through a nasal tube to the stomach or small
intestine. Tube feeding is particularly useful in patients with swallowing
difficulties or anorexia. During tube feeding, liquid may be pumped
continuously at a constant rate of 75 to 150 cm3 per hour for 8–24
h. Liquid foods for tube feeding are available commercially as formulae that
meet nearly all the patient needs. In some cases, food is administered as a
bolus, that is, infusing a discrete volume of formula through the tube under
gravity several times daily. It has the advantages of reducing the cost and
allowing stable long-term patients more mobility. Parenteral feeding bypasses
the GIT so nutrients are delivered directly into the blood. It is only used
when oral or tube feeding have been deemed unsuitable; such as in patients who
cannot eat or absorb food from the GIT. Total parenteral nutrition given via
the peripheral veins or, in cases of long-term nutrition, through a central
venous catheter can provide complete nutrition using preparations containing
appropriate amounts of energy, amino acids, vitamins, minerals and trace
elements. Like liquid foods for tube feeding, these preparations are available
commercially but they are occasionally prepared individually to meet a
patient’s specific needs. Patients on long-term total parenteral nutrition
require careful clinical and laboratory monitoring. Indeed, patients often have
an increased risk of infection at the venous catheter site so care is
necessary. Biochemical changes usually precede any clinical signs of nutrient
deficiency and so regular laboratory monitoring is essential for early
detection of any micronutrient deficiency.

Patients with PEM cannot immediately accept normal food because
there are digestive enzyme deficiencies and often gastroenteritis. Rehydration
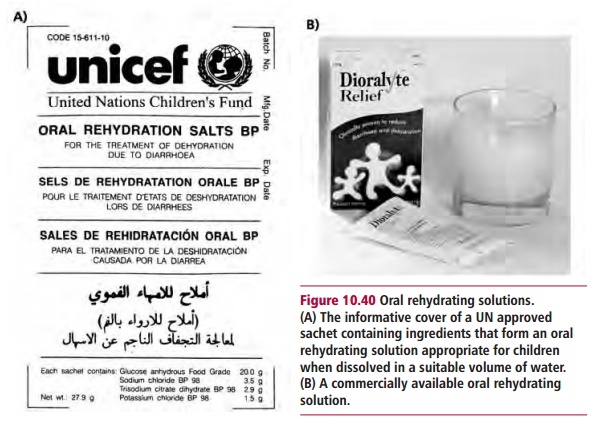
is a priority and oral solutions (Figure
10.40) achieve this in some cases, while intravenous infusions may be
necessary in severe cases. Diluted milk with added sugar may be given initially
and as this becomes accepted the proportion of milk can be gradually increased.
The cessation of diarrhea indicates that the health of the GIT mucosa is
improving and normal foods can be gradually returned to the diet.
The management of obesity aims to reduce food intake,
particularly total energy intake, and to encourage regular exercise. This is
often achieved by cutting down on high energy foods, such as fats and alcohol.
Education and psychological support can be helpful in cases of severe obesity.
Orlistat, an inhibitor of pancreatic lipase, has been used to manage obesity
since it reduces the digestion and absorption of dietary fats and sibutramine
to suppress the appetite, in conjunction with an energy-controlled diet, has
been used to control weight. Surgery is used in some cases of severe obesity.
Jejuno-ileal bypass surgery for morbid obesity was first performed in 1952. In
this process the end of the jejunum or the beginning of the ileum are removed
and the remaining portions joined together. Most of the small intestine is
removed leaving only a short length for digestion and absorption. Although
jejuno-ileal bypass surgery results in a very good weight loss, severe side
effects occur. The technique has been replaced with gastric bypass surgery
where the upper part of the stomach is connected to the small intestine about
one third of the way along its length. Thus only the lower part of the stomach
and approximately two thirds of the small intestine are available for digestion
and absorption, reducing energy intake and therefore weight, but dieting is
still likely to be required. Again, this operation is not without the risk of
developing serious postoperative complications. Liposuction may also be used to
remove fat from under the skin though this is typically performed mainly for
cosmetic rather than therapeutic reasons.
Eating disorders, such as AN and BN, are difficult to prevent
and remain hard to treat. There are seemingly few effective treatments and no
universally recognized plan of treatment. However, the goals of any therapy
must be to establish normal eating patterns and to restore the patient’s
nutritional status and weight. Usually a multidisciplinary approach tailored to
the individual is used. This will involve specialists in nutrition and mental
health in addition to clinicians. Therapy generally involves the family,
behavior modification and nutrition counseling, support groups and the use of
antidepressants. Most patients with AN or BN are treated as outpatients
although in severe cases hospitalization may be necessary. Given that
compliance is often problematic, AN and BN are generally considered to be
chronic disorders interrupted only by intermittent periods of short-lived
remission.
Related Topics