Chapter: Basic & Clinical Pharmacology : General Anesthetics
Etomidate - Intravenous Anesthetics
ETOMIDATE
Etomidate
(Figure 24–6) is an intravenous anesthetic with hypnotic but not analgesic
effects and is often chosen for its minimal hemodynamic effects. Although its
pharmacokinetics are favorable, endocrine side effects limit its use for
continuous infusions. Etomidate is a carboxylated imidazole derivative that is
poorly soluble in water and is therefore supplied as a 2 mg/mL solution in 35%
propylene glycol. The solution has a pH of 6.9 and thus does not cause problems
with precipitation as thiopen-tal does. Etomidate appears to have GABA-like
effects and seems to act primarily through potentiation of GABAA-mediated
chloride currents, like most other intravenous anesthetics.
Pharmacokinetics
An
induction dose of etomidate produces rapid onset of anesthesia, and recovery
depends on redistribution to inactive tissue sites, comparable to thiopental
and propofol. Metabolism is primarily by ester hydrolysis to inactive
metabolites, which are then excreted in urine (78%) and bile (22%). Less than
3% of an administered dose of etomidate is excreted as unchanged drug in urine.
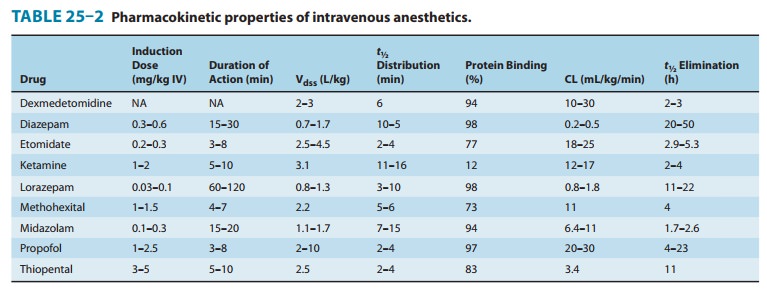
Clearance of etomidate is about five times that of thiopental, as reflected by
a shorter elimination half-time (Table 25–2). The duration of action is
linearly related to the dose, with each 0.1 mg/kg providing about 100 seconds
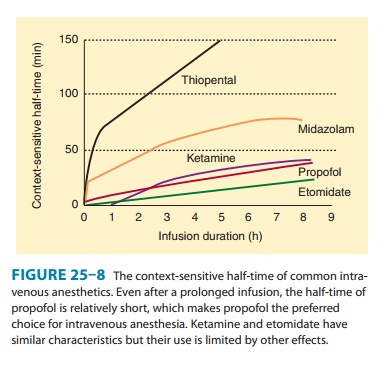
of unconsciousness. Because of etomidate’s minimal effects on hemodynamics and
short context-sensitive half-time, larger doses, repeated boluses, or
continuous infusions can safely be administered. Etomidate, like most other
intravenous anesthetics, is highly protein bound (77%), primarily to albumin.
Organ System Effects
A. CNS Effects
Etomidate
is a potent cerebral vasoconstrictor, as reflected by decreases in cerebral
blood flow and ICP. These effects are similar to those produced by comparable
doses of thiopental. Despite its reduction of CMRO2, etomidate has
failed to show neuroprotective properties in animal studies, and human studies
are lacking. The frequency of excitatory spikes on the EEG after the
administration of etomidate is greater than with thiopental. Similar to
metho-hexital, etomidate may activate seizure foci, manifested as fast activity
on the EEG. In addition, spontaneous movements charac-terized as myoclonus
occur in more than 50% of patients receiving etomidate, and this myoclonic
activity may be associated with seizure-like activity on the EEG.
B. Cardiovascular Effects
A
characteristic and desired feature of induction of anesthesia with etomidate is
cardiovascular stability after bolus injection. In this regard, decrease in
systemic blood pressure is modest or absent and principally reflects a decrease
in systemic vascular resistance. Therefore, the systemic blood
pressure-lowering effects of etomidate are probably exaggerated in the presence
of hypo-volemia, and optimization of the patient’s intravascular fluid volume
status before induction of anesthesia should be achieved.
Etomidate
produces minimal changes in heart rate and cardiac output. Its depressant
effects on myocardial contractility are minimal at concentrations used for
induction of anesthesia.
C. Respiratory Effects
The
depressant effects of etomidate on ventilation are less pro-nounced than those
of barbiturates, although apnea may occasion-ally follow rapid intravenous
injection of the drug. Depression of ventilation may be exaggerated when
etomidate is combined with inhaled anesthetics or opioids.
D. Endocrine Effects
Etomidate
causes adrenocortical suppression by producing a dose-dependent inhibition of
11β-hydroxylase,
an enzyme necessary for the conversion of cholesterol to cortisol. This
suppression lasts 4–8 hours after an induction dose of the drug. Despite
concerns regarding this finding, no outcome studies have demonstrated an
adverse effect. However, because of its endocrine effects, etomi-date is not
used as continuous infusion.
Clinical Uses & Dosage
Etomidate
is an alternative to propofol and barbiturates for the rapid intravenous
induction of anesthesia, especially in patients with compromised myocardial
contractility. After a standard induction dose (0.2–0.3 mg/kg IV), the onset of
unconsciousness is comparable to that achieved by thiopental and propofol.
Similar to propofol, during intravenous injection of etomidate there is a high
incidence of pain, which may be followed by venous irritation. Involuntary
myoclonic movements are also common but may be masked by the concomitant
administration of neuromuscular blocking drugs. Awakening after a single
intra-venous dose of etomidate is rapid, with little evidence of any residual
depressant effects. Etomidate does not produce analgesia, and postoperative
nausea and vomiting may be more common than after the administration of thiopental
or propofol.
Related Topics