Chapter: Basic & Clinical Pharmacology : General Anesthetics
Benzodiazepines - Intravenous Anesthetics
BENZODIAZEPINES
Benzodiazepines
commonly used in the perioperative period include midazolam, lorazepam, and
less frequently, diazepam. Benzodiazepines are unique among the group of
intravenous anes-thetics in that their action can readily be terminated by
adminis-tration of their selective antagonist, flumazenil. Their most desired
effects are anxiolysis and anterograde amnesia, which are extremely useful for
premedication.
Pharmacokinetics in the Anesthesia Setting
The
highly lipid-soluble benzodiazepines rapidly enter the CNS, which accounts for
their rapid onset of action, followed by redis-tribution to inactive tissue
sites and subsequent termination of the drug effect.
Despite
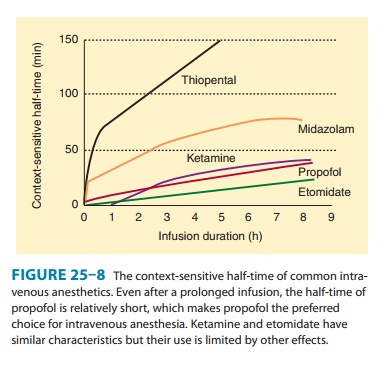
its prompt passage into the brain, midazolam is con-sidered to have a slower
effect-site equilibration time than propo-fol and thiopental. In this regard,
intravenous doses of midazolam should be sufficiently spaced to permit the peak
clinical effect to be recognized before a repeat dose is considered. Midazolam
has the shortest context-sensitive half-time, which makes it the only one of
the three benzodiazepine drugs suitable for continuous infusion (Figure 25–8).
Organ System Effects
A. CNS Effects
Similar
to propofol and barbiturates, benzodiazepines decrease CMRO2 and
cerebral blood flow, but to a smaller extent. There appears to be a ceiling
effect for benzodiazepine-induced decreases in CMRO2 as evidenced by
midazolam’s inability to produce an isoelectric EEG. Patients with decreased
intracranial compliance demonstrate little or no change in ICP after the administration
of midazolam. Although neuroprotective properties have not been shown for
benzodiazepines, these drugs are potent anticonvulsants used in the treatment
of status epilepticus, alcohol withdrawal, and local anesthetic-induced
seizures. The CNS effects of benzodiazepines can be promptly terminated by
administration of the selective benzodiazepine antagonist flumazenil, which
improves their safety profile.
B. Cardiovascular Effects
If
used for the induction of anesthesia, midazolam produces a greater decrease in
systemic blood pressure than comparable doses of diazepam. These changes are
most likely due to peripheral vaso-dilation inasmuch as cardiac output is not
changed. Similar to other intravenous induction agents, midazolam’s effect on
sys-temic blood pressure is exaggerated in hypovolemic patients.
C. Respiratory Effects
Benzodiazepines
produce minimal depression of ventilation, although transient apnea may follow
rapid intravenous administration of midazolam for induction of anesthesia,
especially in the presence of opioid premedication. Benzodiazepines decrease
the ventilatory response to carbon dioxide, but this effect is not usually
significant if they are administered alone. More severe respiratory depression
can occur when benzodiazepines are administered together with opioids. Another
problem affecting ventilation is airway obstruction induced by the hypnotic
effects of benzodiazepines.
D. Other Effects
Pain
during intravenous and intramuscular injection and subse-quent thrombophlebitis
are most pronounced with diazepam and reflect the poor water solubility of this
benzodiazepine, which requires an organic solvent in the formulation. Despite
its better solubility (which eliminates the need for an organic solvent),
midazolam may also produce pain on injection. Allergic reactions to benzodiazepines
are rare to nonexistent.
Clinical Uses & Dosage
Benzodiazepines
are most commonly used for preoperative medi-cation, intravenous sedation, and
suppression of seizure activity. Less frequently, midazolam and diazepam may
also be used to induce general anesthesia. The slow onset and prolonged
duration of action of lorazepam limit its usefulness for preoperative
medica-tion or induction of anesthesia, especially when rapid and sus-tained
awakening at the end of surgery is desirable. Although flumazenil (8–15 mcg/kg
IV) may be useful for treating patients experiencing delayed awakening, its
duration of action is brief (about 20 minutes) and resedation may occur.
The
amnestic, anxiolytic, and sedative effects of benzodiaz-epines make this class
of drugs the most popular choice for preop-erative medication. Midazolam (1–2
mg IV) is effective for premedication, sedation during regional anesthesia, and
brief therapeutic procedures. Midazolam has a more rapid onset, with greater
amnesia and less postoperative sedation, than diazepam. Midazolam is also the
most commonly used oral premedication for children; 0.5 mg/kg administered
orally 30 minutes before induction of anesthesia provides reliable sedation and
anxiolysis in children without producing delayed awakening.
The synergistic effects between benzodiazepines and other drugs, especially opioids and propofol, can be used to achieve bet-ter sedation and analgesia but may also greatly enhance their combined respiratory depression and may lead to airway obstruc-tion or apnea. Because benzodiazepine effects are more pro-nounced with increasing age, dose reduction and careful titration may be necessary in elderly patients.
General
anesthesia can be induced by the administration of midazolam (0.1–0.3 mg/kg
IV), but the onset of unconsciousness is slower than after the administration
of thiopental, propofol, or etomidate. Delayed awakening is a potential
disadvantage, limiting the usefulness of benzodiazepines for induction of
general anesthe-sia despite their advantage of less pronounced circulatory
effects.
Related Topics