Chapter: Surgical Pathology Dissection : The Digestive System
Esophagus: Surgical Pathology Dissection
Esophagus
Esophagectomies
Esophagectomies
are almost always performed to resect neoplastic processes. The nature and
extent of the neoplastic process, however, may be quite variable. Lesions may
range from micro-scopic alterations in patients with a long history of
Barrett’s esophagus to large fungating carcino-mas in patients presenting with
obstruction and dysphagia.
Esophagectomy
specimens (either segmental esophagectomy or esophagogastrectomy) are
ana-tomically simple structures consisting essentially of a straight muscular
tube. Orientation is seldom difficult, since a cuff of stomach is usually
re-sected in continuity with the distal portion of esophagus. After measuring
the dimensions of the specimen, ink its outer surface and the mucosal margins.
The esophagus, you will recall, does not have a serosa. Rather, the surface of
the soft tis-sues investing the esophagus represents a true soft tissue margin.
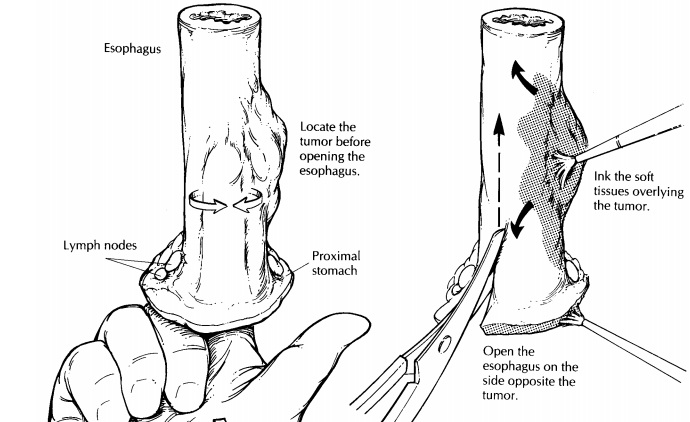
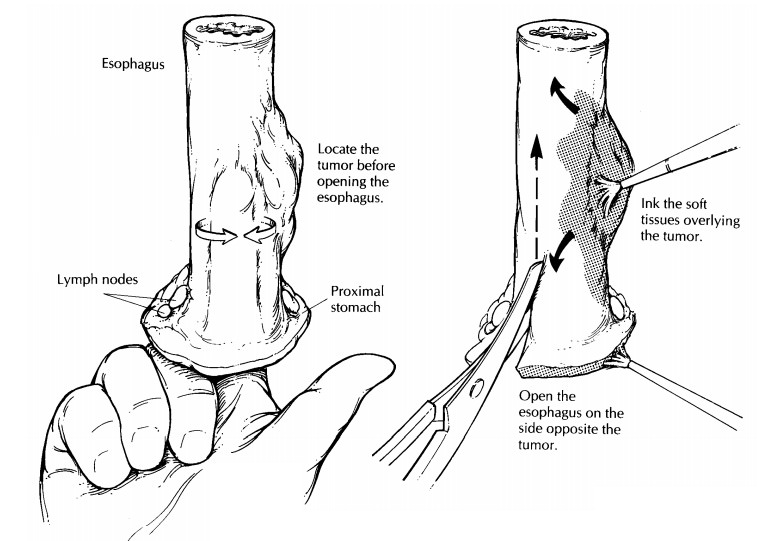
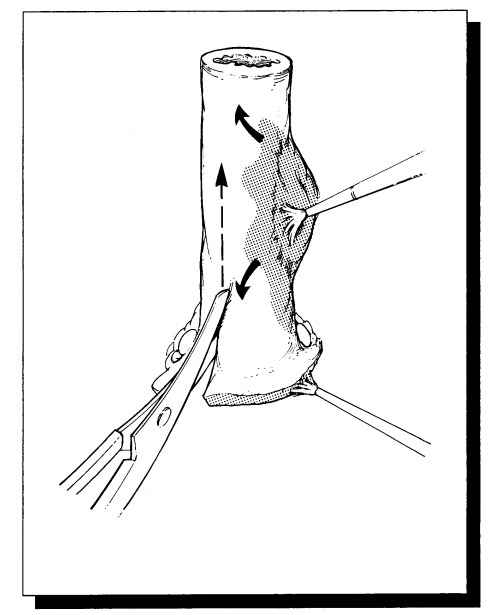
Next,
open the esophagus to expose the muco-sal surface. As illustrated, this step
involves cut-ting through the wall of the esophagus from one end of the specimen
to the other. A common mistake is to cut directly across the tumor. This can be
a costly error, since it distorts the appear-ance of the tumor and disrupts the
tumor’s rela-tionship with underlying structures. Fortunately, this can easily
be avoided by first localizing the tumor and then cutting through the
esophageal wall on the opposite side. The key, of course, is to pay close
attention to the location of the tumor before heedlessly wielding the scissors.
Begin by palpating the unopened esophagus. Areas of in-duration often divulge
the location and extent of an infiltrating tumor. Next, cut the esophagus in a
stepwise fashion: Inspect the lumen with a probing finger, and then advance the
scissors one cautious cut at a time.
Once the
specimen is opened, observe the ap-pearance and thickness of the esophageal
wall. If strictures are present, measure the luminal cir-cumference of the
esophagus at the point of narrowing and at the point of maximal dilatation
proximal to the stricture. Carefully inspect the mucosa. If a tumor is not
seen, try to identify the site of a previous biopsy. Biopsy site changes can be
subtle. Look for focal areas of mucosal hemorrhage, ulceration, scarring, and
puckering. Identify the gastroesophageal junction (GEJ), the point at which the
tubular esophagus joins the saccular stomach. It is usually located 1 to 2 cm
from the proximal edges of the gastric folds. Keep in mind that the GEJ does
not always correlate with the squamocolumnar mucosal junction. Rather, the
squamocolumnar junction normally may occur anywhere within the distal 2 to 3 cm
of esophagus. The gastric mucosa is velvety red, and it contrasts sharply with
the smooth gray appearance of the squamous epithelium lining the esophagus.
Proximal extension of the squa-mocolumnar junction beyond the distal 2 to 3 cm
of the esophagus is abnormal and suggestive of Barrett’s esophagus.
If a
tumor is apparent, note its dimensions (give three dimensions) and its location
with respect to the squamocolumnar and gastroesophageal junctions. Note the
configuration of the tumor (exophytic/fungating, endophytic/ulcerating,
dif-fuse infiltrative).
If the
tumor is at the gastroesophageal junction, it is classified as esophageal if
the epicenter is in the esophagus, as gastric if the epicenter is in
This
distinction is of clinical significance, as stag-ing criteria differ according
to the site: The AJCC staging system recognizes N0 and NI for esopha-geal
cancers, whereas N0, N1, N2 and N3 desig-nations are used for staging gastric
cancers.
The
following should be noted: (1) the propor-tion of tumor located in the
esophagus versus that in the stomach; (2) the greatest dimensions of each
individual component; (3) the anatomic site of the center of the tumor. (If
more than 50% of the tumor involves the esophagus, the tumor is staged as esophageal,
whereas if more than 50% involves the stomach, the tumor is staged as
gas-tric.); and 4) the distance of the tumor’s edges from the margins of
resection. The distance of the tumor to the resection margin should always be
measured in the fresh specimen; fixation causes the mucosa to retract, giving
the appear-ance that the mucosal margins are closer to the tumor than they
actually are. Photograph the opened specimen to document the gross findings.
Before placing the specimen in formalin, ask yourself if fresh tissue should be
submitted for special studies. Pin the specimen flat onto a wax tablet, and
submerge it in formalin until well fixed.
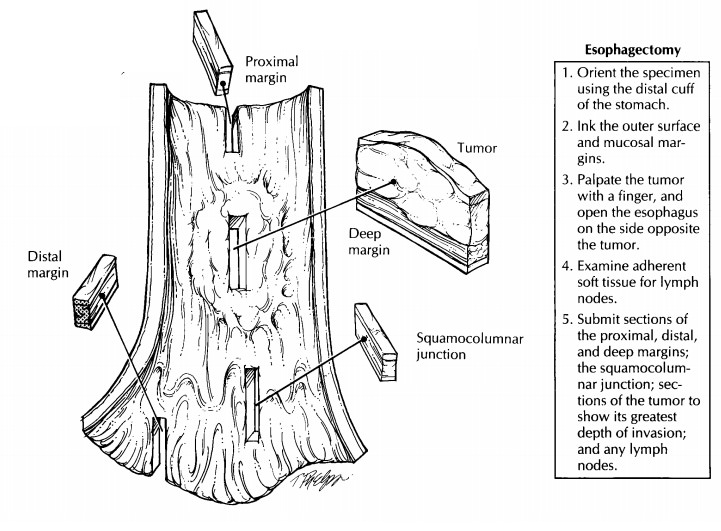
Once the
specimen is fixed, section through the full thickness of the tumor and the
underlying wall to determine the level and depth of tumor extension. Submit at
least two full-thickness sec-tions of the esophagus at the level where it
ap-pears most deeply penetrated by the tumor. Be sure that these sections
include the inked soft tissue surface (radial margin) so that this margin can
be assessed. Also take sections of tumor to demonstrate its relationship to the
adjacent mucosa, and liberally sample areas of Barrett’s mucosa. In those cases
where a tumor is not grossly apparent, three specific areas should be entirely
submitted for histologic evaluation:
(1)
the squamocolumnar junction; (2) areas of
ab-normal mucosa such as the red velvety changes seen in Barrett’s mucosa; and
(3) previous biopsy sites. Sample the proximal and distal resection margins
using perpendicular sections if the tumor is close or shave sections if the
tumor is far removed.
Carefully
dissect the soft tissues investing the esophagus for lymph nodes. Most of these
lymph nodes will be found in the region of the gastro-esophageal junction.
Submit each lymph node found for histologic evaluation.
Important Issues to Address in Your Surgical Pathology Report on Esophagectomies
· What
procedure was performed, and what structures/organs are present?
·
In which portion of the esophagus does the
tumor arise (cervical, upper thoracic, midtho-racic, lower thoracic)?
· What are
the histologic type and grade of the tumor?
·
What are the size, location, and depth of
max-imum invasion of the tumor? Is it in
situ? If invasive, into which level does it invade (lamina propria or
submucosa, muscularis pro-pria, adventitia, or adjacent structures)?
·
Is there invasion into the stomach? Is there
lym-phatic/vascular space invasion?
·
Does the tumor involve any resection margins?
Specifically, what is the status of the proxi-mal (esophageal), distal
(stomach), and deep (radial) margins.
·
What is the condition of the non-neoplastic/
preneoplastic esophagus? For example, are there changes of Barrett’s esophagus,
dyspla-sia, inflammation, or infection?
·
Is there evidence of metastatic disease? Record
the number of lymph nodes examined and the number of lymph node metastases.
Related Topics