Chapter: Surgical Pathology Dissection : The Digestive System
Resections of Intestinal Neoplasms: Surgical Pathology Dissection
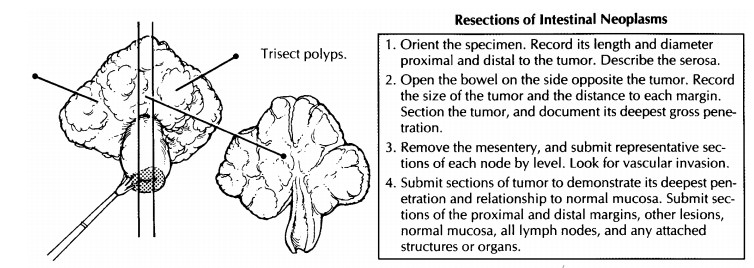
Resections of Intestinal Neoplasms
The
pathologic evaluation of resected intestinal neoplasms plays an integral part
in determining the patient’s prognosis and in selecting the appro-priate
adjuvant therapy. As is true for other specimens, a systematic approach to
your dissection is the best way to ensure that all of the appropriate
information is included in your final report.
Start
with the patient’s history. This should include both the patient’s clinical
history (Crohn’s disease, ulcerative colitis, polyps, family history) and the
relevant endoscopic findings. Next, iden-tify the segment of bowel that was
resected, and orient the specimen. As described earily, the large intestine is
readily distinguished from the small intestine by its larger diameter and the
presence of longitudinal muscle bands (the teniae coli), sacculations (the
haustra), and the ap-pendices epiploicae. In addition, the small intes-tine
shows mucosal folds that stretch across the entire circumference of the bowel,
whereas the large intestinal mucosal folds are discontinuous. The rectum can be
distinguished from the colon by the absence of a peritoneal surface covering
the rectum. Record the length and the diameter of the bowel. The diameter
should be recorded both proximal and distal to any lesions. Look for and
document the presence and appearance of any other structures, such as the
appendix. Next, describe the serosa. Are any diverticula, gross perforations,
or serosal nodules present?
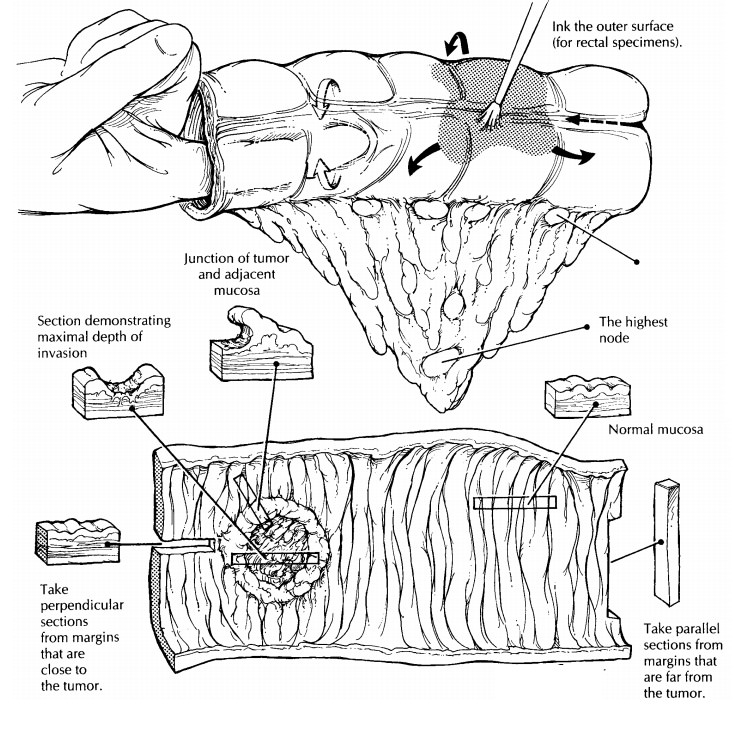
As noted
above, the rectum lacks a serosal lining. Therefore, the outer surface of the
rectum represents a true soft tissue margin, and these soft tissues should be
inked. Otherwise, only the proximal and distal margins need to be inked. When
opening the bowel, make every effort not to cut through the tumor. First,
localize the tumor by palpating the specimen and probing the lumen of the bowel
with your finger, then open the bowel on the side opposite the tumor. If a
tumor cannot be appreciated grossly, simply open the small intestine adjacent
to the mesenvery, the colon along the anterior (free) teniae, and the rectum
along the midline anteriorly. Once the specimen has been opened, gently rinse
off the intestinal contents using a stream of isotonic saline.
Next,
systematically describe the opened speci-men. Start with the tumor. Document
its location relative to the margins and to any landmarks, such as the
ileocecal valve or the pectinate line.
Describe
the size of the tumor in its longitudinal and transverse dimensions, as well at
its gross configuration (endophytic, pedunculated, sessile, diffusely
infiltrative, or annular). It is especially critical to document tumor size for
anal carcino-mas, since it is tumor size rather than depth of invasion that
serves as the key feature for as-sessing ‘‘T’’ when staging the tumor. Multiple
cancers should be looked for, described, and labeled separately. After the
tumor has been described, make multiple parallel 2- to 3-mm sec-tions through
the tumor, and note its deepest gross penetration. It is also important to note
if bowel perforation (a hole in the bowel wall) is associated with the tumor.
Also note the distance from the tumor to the soft tissue or radial margin. This is the distance from
the outermost part of the tumor to the lateral margin of resection along a
radius drawn from the center of the lumen of the bowel through the deepest
penetration of the tumor. The soft tissue margin is only important for rectal
cancers and for colon cancers located on the mesenteric aspect of the bowel.
![]()
After
the tumor has been described, turn your attention to the remainder of the
bowel. Be sys-tematic in your description. For example, begin with the mucosa,
wall, and serosa of the proximal portion of the specimen and then proceed dis-tally.
When describing the mucosa, note diverti-cula, changes of inflammatory bowel
disease, polyps, and ischemic changes. A systematic ap-proach to your gross
dictation will ensure that all important findings are included.
We like
to examine the soft tissues for lymph nodes in the fresh state because the
nodes are easier to palpate and because they retain their pink color, which
contrasts to the yellow fat. The next step, therefore, is to dissect the
mesentery. Look for and sample any lymph nodes adjacent to the point of
ligation of the vascular pedicle, and designate these as the highest lymph
nodes. Next, cut the mesentery close to the bowel, main-taining anatomic
orientation. Do not remove any areas in which the tumor directly extends into
the mesenteric fat. Sample these as a part of the deep margin after the
specimen has been fixed. Then divide the detached mesenteric fat into groups:
those proximal to the tumor, those at the level of the tumor, and those distal
to the tumor. If any great vessels are present, identify and sepa-rately
designate the nodes adjacent to them. Thinly section the mesenteric fat at each
level, and examine and palpate each section for lymph nodes. Submit for
histology each identified node. When looking for the nodes, remember that they
are frequently present at the junction of the bowel wall and the mesentery.
When submitting the lymph nodes for histologic processing, remember to
designate the level from which they were taken. Also examine the veins and
arteries in the mesentery for thrombi. If any are present, submit a
representative section of the involved vessel for histologic examination. After
the mesentery has been examined, separately bundle each level for fixation and
storage. Should you ever have to return to the mesentery, the orientation will
be preserved. The specimen can now be pinned to a wax tablet and fixed
overnight.
After
the specimen is well fixed, it can be sampled. Start with the tumor. Submit at
least two sections: one from the edge of the tumor to show the junction of
tumor and normal bowel, and one from the point of deepest tumor penetration
into the wall of the bowel. If the tumor does not grossly appear to involve the
bowel wall, then submit the entire base of the lesion to demonstrate the
presence or absence of invasion.
Submit
the proximal and distal margins. If the tumor is close to a margin, these
sections should be perpendicular (longitudinal), and if the tumor is far from a
margin, these sections can be parallel (transverse). Next, sample any other
lesions.
When sampling polyps, remember to include both the head and stalk in your sections. Submit representative sections of normal bowel mucosa and wall, and submit representative sections of all remaining structures/organs, such as the appendix and terminal ileum. Remember that longitudinal sections are better than transverse sections when sampling the colon wall.
Important Issues to Address in Your Surgical Pathology Report on Resections for Intestinal Neoplasms
·
What procedure was performed, and what
structures/organs are present?
·
What is the location of the tumor?
·
What are the dimensions of the tumor?
·
What is the gross configuration of the tumor
(endophytic, pedunculated, sessile, diffusely infiltrating, annular)?
·
What are the histologic type and grade of the
neoplasm?
·
What is the maximum depth of invasion of the
tumor? Is it in situ (high-grade dysplasia), or does it extend into the lamina
propria, sub-mucosa, muscularis propria, or through the muscularis propria into
subserosa? Does the tumor extend into other organs, or does it ex-tend into the
visceral peritoneum?
·
Is there bowel wall perforation?
·
Is any vascular invasion identified?
·
What is the status of the margins (proximal,
distal, and radial)?
·
How many lymph node metastases were identified,
and how many lymph nodes were sampled at each level?
·
Are there mesenteric deposits? For staging
purposes, tumor nodules in the pericolorectal fat without histologic evidence
of residual lymph node are classified as regional node metastases
·
if they have the form and smooth contour of a
lymph node. Nodules with irregular contours are believed to reflect microscopic
venous invasion using AJCC criteria.
·
Are any other lesions noted (e.g., adenomas,
intestinal inflammatory disease, dysplasia)?
Related Topics