Chapter: Surgical Pathology Dissection : The Digestive System
Stomach: Surgical Pathology Dissection
Stomach
Total and Partial Gastrectomies
Stomach
specimens come in a variety of shapes and sizes depending on the pathologic
process for which the stomach is removed. For example, a small portion of
stomach may be removed for peptic ulcer disease, while the entire stomach and
even adjacent organs can be resected when an infiltrating cancer is present.
Regardless of the specimen’s size and shape, a wise approach is to regard every
stomach resection as though it potentially harbors a malignant neoplasm. Do not
be betrayed by the innocent-looking ulcer. Instead, take care to evaluate the
resection mar-gins, adequately sample the lesion, and diligently search for
lymph nodes. With this approach, the dissection should always be adequate, even
in that rare instance when a carcinoma is incidentally discovered in a
benign-appearing ulcer.
The
dissection of a stomach specimen begins with a basic understanding of the stomach’s
anat-omy. This understanding is important for two reasons: First, the anatomic
regions of the stom-ach are functionally and histologically distinct; thus,
each region of the stomach should be indi-vidually assessed. Second, anatomic
landmarks can be used to orient most stomach specimens. The four divisions of
the stomach are the cardia, fundus, body, and antrum. The cardia is the rim of
the stomach that surrounds the gastroesopha-geal junction (GEJ). The fundus is
the dome-shaped region of the stomach that sweeps superior to the GEJ. The body
accounts for the major portion of the stomach. It narrows distally as it merges
with the antrum. The antrum is the distal third of the stomach and includes the
pyloric sphincter. The anatomic boundaries separating these regions are not
distinct, at least not in the unopened specimen. Once the mucosal surface is
exposed, however, the demarcation between the body and antrum can be easier to
appreciate. For example, the body shows prominent rugal folds, whereas the mucosa
of the antrum is compara-tively flat. This flattened antral surface forms a V.
The nadir of the V rests on the lesser curvature and points toward the proximal
portion of the stomach. Other landmarks that are useful in ori-enting the
specimen include the greater curva-ture, the broad and convex inferior aspect
of the stomach; the lesser curvature, the concave su-perior aspect of the
stomach; and the pyloric ring, a thick muscular collar at the outlet of the
stom-ach. In more limited stomach resections, these landmarks may not be
present and correct orien-tation relies upon the surgeon’s designation.
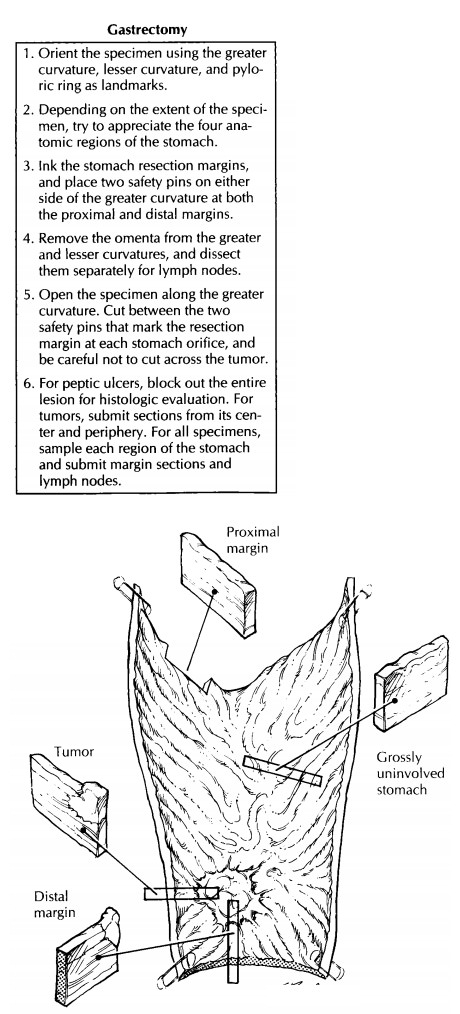
Begin
your examination by clearly marking the stomach resection margins. Keep in mind
that these margins may be difficult to reconstruct once the specimen has been
opened. One simple method is to ink the margins and then place four safety
pins—two on either side of the greater curvature at both the proximal and
distal mar-gins. By cutting the specimen between these safety pins, you can
easily reconstruct the opened speci-men simply by juxtaposing the two pins.
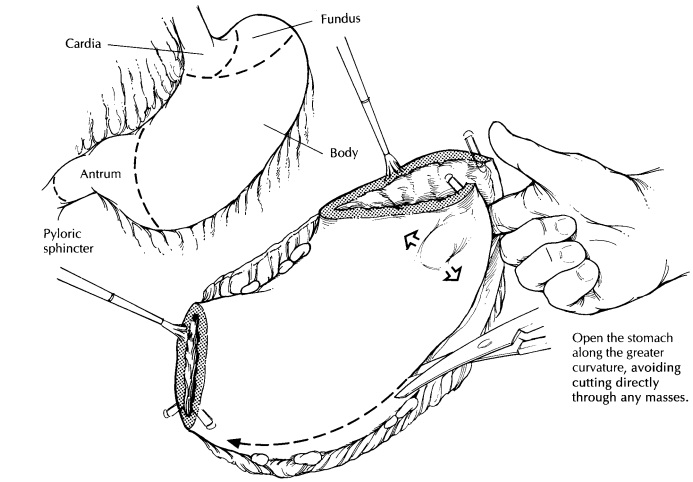
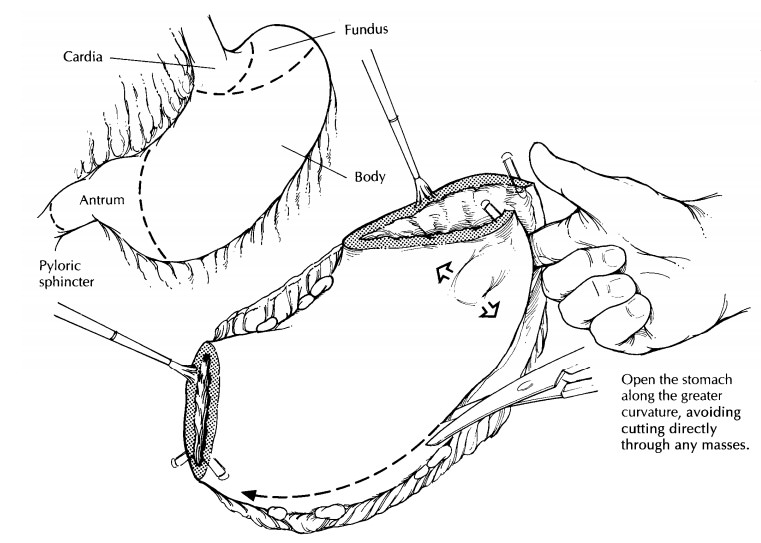
To
facilitate handling of the stomach, remove the bulky omenta (when present)
suspended from the greater and lesser curvatures of the stomach. Do not discard
this fat. Instead, set it aside for later dissection. Next, open the stomach
along its entire length, cutting between the safety pins at each stomach
orifice. To avoid cutting across the lesion, insert a probing finger into the
lumen, and explore the inner surface of the stomach ahead of the advancing
scissors. Be flex-ible in your approach. Whenever possible, cut along the
greater curvature, but always be ready to tailor the dissection to avoid
cutting through a tumor. When the line of excision along the greater curvature
is obstructed by a tumor, the lesser curvature may serve as an alternative
route for opening the stomach.
Once the
stomach is opened, evaluate each of the three layers of the stomach—the mucosa,
wall, and serosa. Do the gastric folds appear thickened or effaced? Assess the
number, size, location, and appearance of any lesions. For ulcer-ative lesions,
carefully note those features that are helpful in distinguishing benign ulcers
(e.g., sharply defined margins, smooth and flat bor-ders, straight walls, clean
base) from gastric carci-nomas (e.g., irregular margins, thickened and
heaped-up borders, shaggy base). Important measurements include not only the
dimensions of the lesion but also the distance from the lesion to the resection
margins. This distance, known as the gross
clearance, should be measured while the specimen is fresh, because the
mucosa tends to retract during fixation.
The
precise location of the tumor should be documented. For tumors involving the
gastro-esophageal junction, every effort should be made to assign a precise
site of origin. The gastroesoph-ageal junction is the junction of the tubular
esophagus and saccular stomach regardless of the type of epithelium lining the
esophagus. Assess the proportion of tumor in the esopha-gus versus the stomach
and find the anatomic location of the tumor’s epicenter. If more than 50% of
the tumor involves the esophagus the tumor is classified as esophageal, whereas
it is classified as gastric if more than 50% involves the stomach.
Next,
examine and describe the wall and the serosa of the stomach. Are any mural
nodules noted? Is the wall diffusely thickened or focally indurated? Are any
serosal lesions noted? Is the serosa retracted? Collect fresh tissue samples
for special studies as needed, then pin the specimen flat on a wax tablet, and
submerge it in forma-lin until well fixed.
‘‘Better safe than sorry’’ is a wise policy when sampling the stomach. Consider again the pru-dence of viewing each lesion with the suspicion that it represents a malignant neoplasm. Thor-oughly sample all lesions, evaluate every margin, and diligently search for lymph nodes. For lesions that are clinically believed to be peptic ulcers, submit the entire ulcer in a sequential fashion so that an underlying malignancy is not missed. When a tumor is apparent, section through it to determine whether it extends into or through the stomach wall. Be sure to describe its gross configuration (exophytic/polypoid, infiltrative, diffusely infiltrative, expansile/noninfiltrative, ulcerating, or annular). Submit sections from the center of the tumor to determine its maxi-mum depth of invasion. Also submit sections from the tumor’s periphery to demonstrate the transition between the tumor and the adjacent gastric mucosa. When the stomach appears dif-fusely thickened by an infiltrative process (e.g., linitis plastica) submit sections from all four re-gions of the stomach. Margins should generally be sampled using perpendicular sections when the tumor is close, and shave sections when the tumor is far removed. Submit all lymph nodes. Keep the greater and lesser omental node groups separate. A good place to find lymph nodes is at the point where the omenta attach to the stomach.
The
grossly uninvolved stomach should also be sampled for histologic evaluation.
Depending on the extent of the resection, these sections should represent all
four regions of the stomach, the squamocolumnar junction, and if present the
contiguous esophagus. For extended resections that include adjacent colon,
spleen, liver, and/or pancreas, sections should be taken to determine the
presence of direct tumor extension, tumor metastases, and the adequacy of
surgical excision (i.e., the status of the margins).
Photography
plays an important role in the eval-uation of stomach specimens. Sections taken
for histology can be mapped with considerable detail on Polaroid or digital
photographs of the speci-men. This is a useful method for correlating the
histologic features with the anatomic region of the stomach.
Important Issues to Address in Your Surgical Pathology Report on Gastrectomies
· What
procedure was performed, and what structures/organs are present?
·
What are the location (cardia, fundus, body, or
antrum), size, type, and histologic grade of the neoplasm?
· Is there
invasion into the esophagus or stomach? Is there blood/lymphatic vessel
invasion? Is there perineural invasion?
·
What is the extent of the neoplasm? Specify
into which level of the wall of the stomach the tumor invades (e.g., mucosa,
submucosa, muscularis propria, subserosal soft tissues, or serosa). Does the
tumor extend beyond the serosa to involve adjacent structures?
· Does the
tumor involve the soft tissue and/or mucosal margins? What is the distance of
the mucosal margin from the edge of the tumor?
· What is
the condition of the non-neoplastic stomach (e.g., changes of Helicobacter pylori gas-tritis or
presence of intestinal metaplasia, dysplasia, atrophy, adenomas, or
ulceration)?
·
Is there evidence of metastatic disease? Record
the number of lymph nodes examined and the number of lymph node metastases.
Related Topics