Chapter: Surgical Pathology Dissection : The Digestive System
Gallbladder and Extrahepatic Biliary System: Surgical Pathology Dissection
Gallbladder and Extrahepatic Biliary System
The
biliary system forms a conduit whereby bile produced by hepatocytes is
transmitted to and concentrated in the gallbladder and finally ex-creted into
the duodenum. Bile is first secreted into bile canaliculi, which form the
smallest branches of the biliary system. Canaliculi drain into interlobular
bile ducts, which join to form progressively larger intrahepatic ducts until
the left and right hepatic ducts emerge from the liver in the region of the
porta hepatis. Slightly distal to the porta hepatis, the left and right hepatic
ducts join to form the common hepatic duct. The common hepatic duct is then
joined on its right side by the cystic duct of the gallbladder to form the
common bile duct. The distal common bile duct usually joins with the pancreatic
duct within the head of the pancreas and empties into the duodenum at the
ampulla of Vater. The exact anatomy and lengths of the various extrahepatic
ducts vary among individuals. The common hepatic duct ranges from 1 to 5 cm in
length, the cystic duct from 2 to 6 cm, and the common bile duct from 5 to 10
cm. The usual diameter is 4 to 5 mm for the cystic duct and 5 to 7 mm for the
common bile duct.
Cholecystectomies
The
gallbladder is one of the more frequently encountered specimens in the surgical
pathol-ogy laboratory. It is usually removed for stones and/or an inflammatory
condition, but it rarely does harbor a neoplasm.
The
gallbladder is a saccular structure com-posed of a fundus, body, and neck. It
progres-sively narrows to form the cystic duct. Even though this structural
anatomy is straightfor-ward, take a moment to orient the specimen and identify
a few important features. First, note that the usual gallbladder has two very
different ex-ternal surfaces. One side of the gallbladder is smooth and glistening,
whereas the other is rough. The distinction between these two surfaces is
important. The smooth surface is lined by perito-neum. In contrast, the rough
surface is where the adventitia of the gallbladder has been dissected from the
undersurface of the liver, and it re-presents a surgical margin. (Rarely, a
gallbladder is entirely buried within the liver parenchyma or is attached to
the liver only by a mesentery.) Second, the lymphatics of the gallbladder drain
into a lymph node located along the cystic duct. When present in the specimen,
this cystic duct lymph node can be identified by palpating the soft tissues
investing the cystic duct.
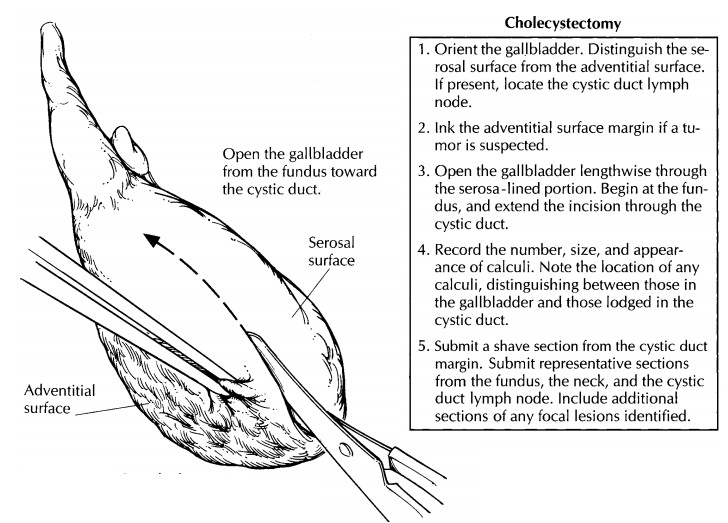
State whether the gallbladder is received fresh or in fixative. Measure the specimen, and describe the external surfaces. One important issue to address at the onset of the dissection is whether the specimen is received intact. Not uncommonly, a gallbladder is opened in the operating room and the stones removed. Receipt of a previously opened gallbladder should be documented in the gross description. If the specimen is still in-tact, open the gallbladder lengthwise through its serosa-lined surface. Using a small pair of scissors, begin at the fundus; next, extend the cut through the body and neck of the gallbladder and then through the cystic duct. The lumen of the cystic duct should be examined, even though the duct may be tortuous and difficult to open. The direction in which the gallbladder is opened is important. Do not begin at the opening of the cystic duct because a probe or scissors forced into this opening could dislodge stones.
After
the specimen has been opened, note the contents of the gallbladder and the
cystic duct. Is the usual thin, dark green bile present; or is it hemorrhagic,
viscous, or sludgy? Is the lumen filled with pus (an infected gallbladder) or
re-placed by clear white mucoid material (muco-cele)? Look for calculi, and
determine whether they are present within the lumen of the gallblad-der or
within the cystic duct. Record the appear-ance of any calculi. Are they round
or faceted? What is their color? Use a sharp blade to cut the calculi in half,
and note the appearance of their cut surfaces. How many calculi are present?
When numerous calculi are present, there is a tendency to record the size of
the largest one. In-stead, record the full range of sizes, keeping in mind that
the smaller calculi are more apt to become lodged in the cystic duct than are
the larger ones.
Next,
measure the thickness of the gallbladder wall, and describe the appearance of
the mucosa. The mucosa is normally bile-stained and has a fine, honeycombed
appearance. A frequent mucosal abnormality is cholesterolosis, in which there
are numerous yellow punctate deposits or interlacing linear yellow streaks on
the mucosa (“strawberry gallbladder”). If a neoplasm is sug-gested by the
presence of an exophytic or ulcera-tive lesion, the external adventitial
surface should be inked, as it represents an important surgical margin.
Describe the location of the neoplasm, its dimensions, and its configuration
(e.g., exo-phytic, ulcerating, diffusely infiltrating with as-sociated wall
thickening). If liver parenchyma is attached to the adventitial surface of the
gall-bladder, does the tumor appear to invade the liver?
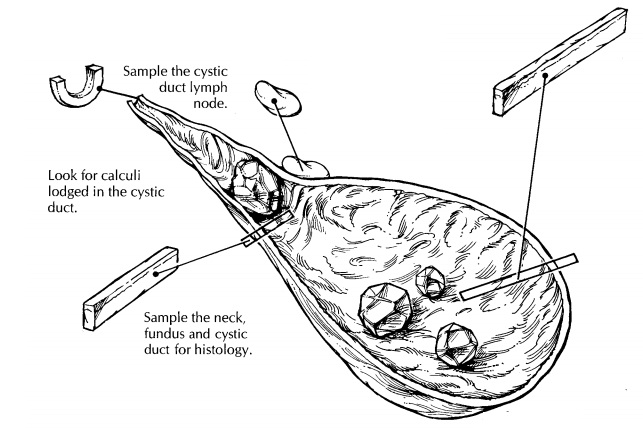
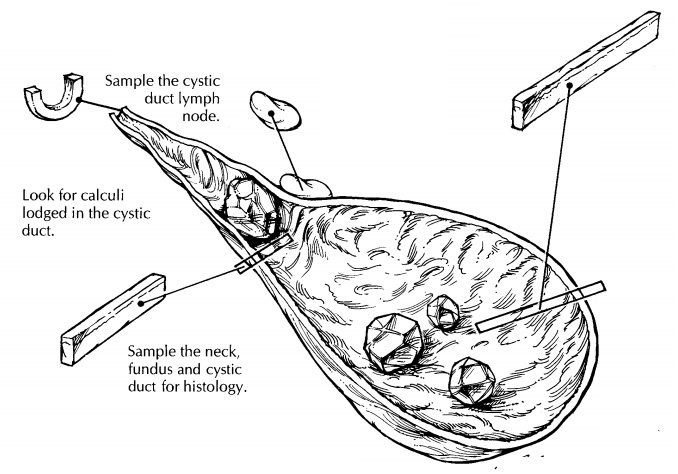
The
gallbladder is best sampled after it has been allowed to fix. For routine
specimens, submit one representative full-thickness section from the fundus,
one through the body/neck of the gallbladder, and one cross section of the
cystic duct margin. Additional sections are required when focal lesions are
present. If a neoplastic process is suspected, obtain full-thickness sec-tions
of the tumor to demonstrate its maximum depth of invasion. Also submit sections
from the periphery of the tumor to demonstrate its relationship to the
surrounding uninvolved mucosa. To assess the status of the margins when a
neoplasm is suspected, submit a shave section from the cystic duct margin and
perpendicular sections from the inked adventitial surface. When present, the
cystic duct lymph node should always be submitted for histologic evaluation.
Local or Segmental Biliary Resections
The
extrahepatic bile ducts are most commonly encountered as part of a
pancreaticoduodenec-tomy (including the distal common bile duct) and partial or
total hepatectomy (including portions of the proximal extrahepatic biliary
tree). Exami-nation of the bile ducts in these specimens is described elsewhere
in this book. Local or seg-mental resections of the extrahepatic bile ducts are
less common but may be performed for carci-noma of the extrahepatic bile ducts,
isolated stric-tures, or choledochal cysts.
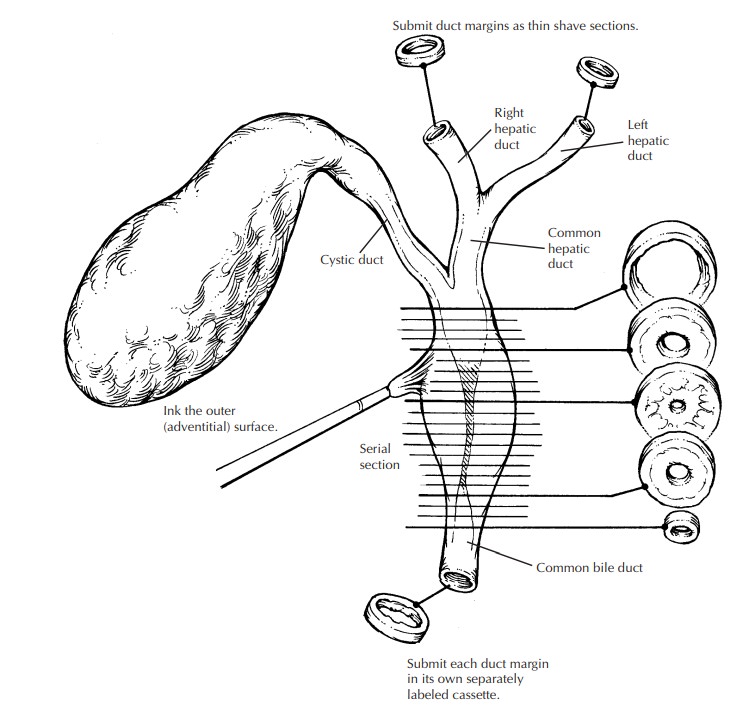
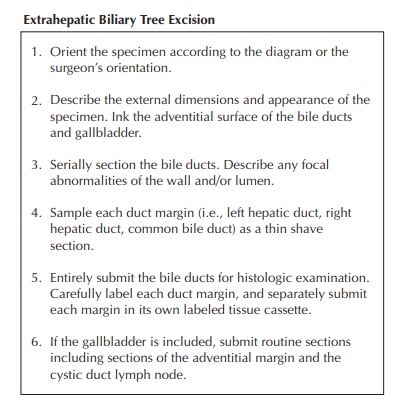
The
specimen should first be oriented, prefera-bly as indicated by the surgeon or
by noting its relationship to the gallbladder. Note if the spec-imen is
received fixed or unfixed, whether it has been previously incised, and whether
other tissues or organs accompany the bile duct. Mea-sure the length and
diameter of each portion of the biliary tree that is present. Describe the
ap-pearance of the external surface, including the presence of any mass lesions
or adhesions. In general, the proximal and distal bile duct margins and the
periductal soft tissue (forming the circumferential margin of the excision)
should then be inked because of the high likelihood of carcinoma.
It is
best not to attempt to open the ducts lon-gitudinally, since small papillary
lesions in the ducts could easily be dislodged and the mucosa disrupted by the
scissors. Instead, make serial cross sections at 2- to 3-mm intervals with a
scalpel, keeping the cross sections oriented with regard to the segment of the
biliary tree and the proximal and distal margins. The resulting cross sections
can then be examined for the presence of any obstructing lesions in the lumen,
the presence of a mass, or the presence of a stricture. If a stric-ture is
present, describe its location and measure its length, the sizes of the bile
duct lumen at, above, and below the stricture, and the thickness of the bile
duct wall in the region of the stricture and elsewhere. Carcinoma of the bile
ducts can infiltrate diffusely into the bile duct wall and thereby mimic a
benign stricture, or it can have a papillary or nodular configuration. If a
calculus, papillary lesion, or mass is seen, describe its loca-tion, whether it
obstructs the lumen, and whether there is obvious penetration of the bile duct
wall and involvement of any adjacent structures. In general, the specimen should
then be submitted in its entirety in serial cross sections, keeping the
proximal and distal shave margins separate. (Surgically resectable carcinomas
of the bile ducts are unlikely to be too large to submit in toto, and segmental
bile duct resections without a grossly obvious tumor would have to be
completely em-bedded anyway.)
Choledochal
cysts should also be inked along the external surface. Measure the dimensions
of the cyst and describe its configuration (e.g., fusi-form or saccular).
Carefully incise the cyst with a scalpel and drain the contents into a
container. Note the volume and type of the fluid present (bile, blood, fibrin,
mucoid material, pus). After draining the cyst contents, open the cyst
longitu-dinally with a small pair of scissors and examine the inner lining.
Specifically, describe the appear-ance of the lining (often denuded,
bile-stained, and shaggy) and the presence of any visible islands of residual
mucosa. Are any masses or suspicious lesions present? The risk of carcinoma
developing within choledochal cysts increases with age, and up to 15% of
choledochal cysts in adults harbor a carcinoma. If a suspicious lesion is
present, describe its dimensions, color, con-sistency, associated necrosis, and
how deeply it penetrates the cyst wall.
Representative
full-thickness sections of the cyst should be taken. They should include
ap-proximately one section per centimeter of cyst wall diameter as well as
proximal and distal shave margins. If any suspicious lesions are pres-ent,
additional sections are needed, including full-thickness sections of the lesion
at its deepest extent and sections that demonstrate the interface between the
lesion and the adjacent cyst wall.
Important Issues to Address in Your Surgical Pathology Report
·
What procedure was performed, and what
structures/organs are present?
·
What are the contents of the gallbladder, bile
duct, or choledochal cyst (e.g., bile, pus, blood, mucus)? When calculi are
present, note their type (pigment, cholesterol, mixed), number, and the range
of sizes. Are any calculi lodged in the cystic duct or present in a bile duct?
·
What are the nature and severity of the
in-flammatory processes (e.g., acute or chronic cholecystitis,
xanthogranulomatous cholecys-titis, primary or secondary sclerosing cholan-gitis)?
For a cholecystectomy, be sure to mention the presence or absence of
perfora-tions and peritonitis.
·
Is a neoplasm present? What are its location,
size, histologic type, histologic grade, and depth of invasion (mucosa,
gallbladder mus-cularis or bile duct fibromuscular layer, peri-muscular or
periductal soft tissue)? Is there angiolymphatic invasion or perineural
inva-sion? Does the tumor extend into adjacent organs? For gallbladder
carcinomas, it is im-portant to note whether there is invasion into the liver,
and whether this invasion is more than 2 cm. Are the adventitial/hepatic bed
margin and the cystic duct margin free of tumor? For bile duct carcinomas, are
the peri-ductal soft tissue margin and the proximal and distal bile duct
margins free of tumor?
·
Are there preneoplastic changes in the
sur-rounding mucosa (intestinal metaplasia, dys-plasia)?
·
How many lymph nodes were examined, and how
many of them harbored a metastasis?
Related Topics