Chapter: Clinical Dermatology: Regional dermatology
Candidiasis
Candidiasis
Cause and presentation
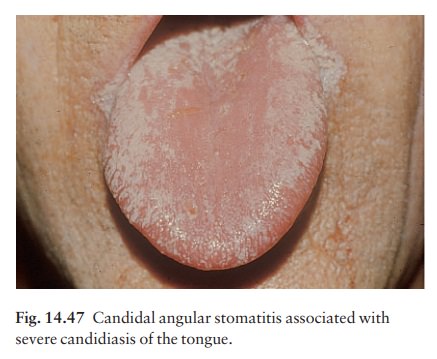
Infections
with Candida
albicans appear suddenly, on the tongue, lips or other mucosae, in
the ‘pseudomem-branous form’ (also called thrush; Fig. 14.47). Small lesions
are more common than large ones. About 15% of infants get thrush on the tongue,
lips or buccal mucosa, often from an infection acquired while pass-ing through
the birth canal. Sometimes candidiasis appears as red sore patches under
dentures, or as angular chelitis (perlèche).
Course
If
the candidiasis is a complication of systemic anti-biotic therapy, treatment
will be curative. Immuno-suppressed and denture-wearing patients often have
recurrent disease.
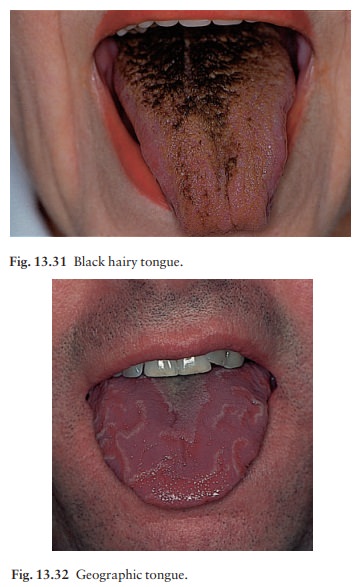
Differential diagnosis
Many tongues are coated with desquamated epithelial cells that create a yellow wet powder on their surface.
This scapes off easily, and
shows no inflammation underneath. Lichen planus, oral hairy leukoplakia and
dysplastic leukoplakia may cause confusion.
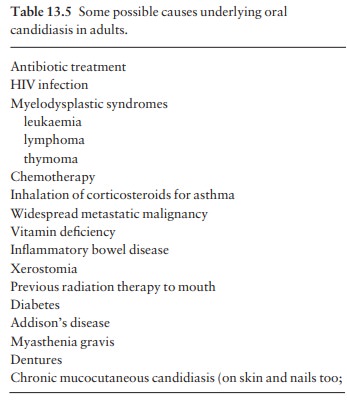
Investigations
Thrush
does not normally occur in healthy adults, in whom the appearance of
candidiasis needs more investigation than just a simple diagnosis by
appear-ance, KOH examination or culture. Table 13.5 lists some possible
underlying causes.
Treatment
Topical
and systemic imidazoles are the treatments of choice. Creams and solutions can
be used, but suck-ing on a clotrimazole troche
three times daily is better. Some patients are best treated with
fluconazole, 150 mg once daily for 1–3 days. If an underlying condition is
present, this should be identified and treated. Patients with ‘denture sore
mouth’ should scrub their dentures each night with toothpaste and a toothbrush,
sleep without dentures, and swish a teaspoonful of nystatin solution around the
dentureless mouth three times a day.
Related Topics