Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Atelectasis
Atelectasis
Atelectasis refers to closure or
collapse of alveoli and often is described in relation to x-ray findings and
clinical signs and symptoms. Atelectasis may be acute or chronic and may cover
a broad range of pathophysiologic changes, from microatelectasis (which is not
detectable on chest x-ray) to macroatelectasis with loss of segmental, lobar,
or overall lung volume. The most commonly described atelectasis is acute
atelectasis, which occurs frequently in the postoperative setting or in people
who are immobilized and have a shallow, monotonous breathing pattern. Excess
secretions or mucus plugs may also cause obstruction of airflow and result in
atelectasis in an area of the lung. Atelectasis also is observed in patients
with a chronic airway obstruction that impedes or blocks air flow to an area of
the lung (eg, obstructive atelectasis in the patient with lung cancer that is
invading or compressing the airways).This type of atelectasis is more insidious
and slower in onset.
Pathophysiology
Atelectasis may occur in the adult as a
result of reduced alveolar ventilation or any type of blockage that impedes the
passage of air to and from the alveoli that normally receive air through the
bronchi and network of airways. The trapped alveolar air becomes absorbed into
the bloodstream, but outside air cannot replace the absorbed air because of the
blockage. As a result, the isolated portion of the lung becomes airless and the
alveoli collapse. This may occur with altered breathing patterns, retained
secretions, pain, alterations in small airway function, prolongedsupine
positioning, increased abdominal pressure, reduced lung volumes due to
musculoskeletal or neurologic disorders, restrictive defects, and specific
surgical procedures (eg, upper abdomi nal, thoracic, or open heart surgery).
Persistent low lung volumessecretions or a mass obstructing or impeding
airflow, and compression of lung tissue may all cause collapse or obstruction
of the airways, which leads to atelectasis.
The postoperative patient is at high
risk for atelectasis because of the numerous respiratory changes that may
occur. A monotonous low tidal breathing pattern may cause airway closure and
alveolar collapse. This results from the effects of anesthesia or analgesic
agents, supine positioning, splinting of the chest wall because of pain, and
abdominal distention. The postoperative patient may also have secretion
retention, airway obstruction, and an impaired cough reflex or may be reluctant
to cough because of pain. Figure 23-1 shows the pathogenic mechanisms and
consequences of acute atelectasis in the postoperative patient.
Atelectasis resulting from bronchial obstruction by secretions may occur in patients with impaired cough mechanisms (eg,postoperative, musculoskeletal or neurologic disorders) or in debilitated, bedridden patients. Atelectasis may also result from excessive pressure on the lung tissue, which restricts normal lung expansion on inspiration. Such pressure may be produced by fluid accumulating within the pleural space (pleural effusion), air in the pleural space (pneumothorax), or blood in the pleural space (hemothorax). The pleural space is the area between the parietal and the visceral pleurae. Pressure may also be produced by a pericardium distended with fluid (pericardial effusion), tumor growth within the thorax, or an elevated diaphragm.
Clinical Manifestations
The
development of atelectasis usually is insidious. Signs and symptoms include
cough, sputum production, and low-grade fever. Fever is universally cited as a
clinical sign of atelectasis, but there are few data to support this. Most
likely the fever that ac-companies atelectasis is due to infection or
inflammation distal to the obstructed airway.
In
acute atelectasis involving a large amount of lung tissue (lobar atelectasis),
marked respiratory distress may be observed. In addition to the above signs and
symptoms, dyspnea, tachycardia, tachypnea, pleural pain, and central cyanosis (a bluish skin hue
that is a late sign of hypoxemia) may be anticipated. The pa-tient
characteristically has difficulty breathing in the supine posi-tion and is
anxious. Signs and symptoms of chronic atelectasis are similar to those of
acute atelectasis. Because the alveolar collapse is chronic, infection may
occur distal to the obstruction. Thus, the signs and symptoms of a pulmonary
infection also may be present.
Assessment and Diagnostic Findings
Decreased
breath sounds and crackles are heard over the affected area. In addition, chest
x-ray findings may reveal patchy infiltrates or consolidated areas. In the
patient who is confined to bed,atelectasis is usually diagnosed by chest x-ray
or identified by physical assessment in the dependent, posterior, basilar areas
of the lungs. Depending on the degree of hypoxemia, pulse oxime-try (SpO2)
may demonstrate a low saturation of hemoglobin with oxygen (less than 90%) or a
lower-than-normal partial pressure of arterial oxygen (PaO2).
Prevention
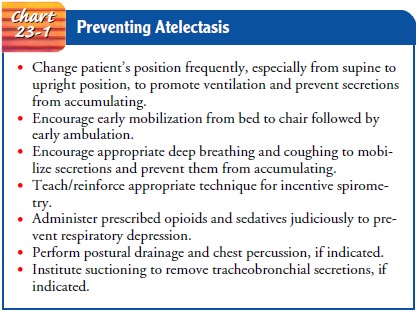
Nursing
measures to prevent atelectasis include frequent turning, early mobilization,
and strategies to expand the lungs and to man-age secretions. Deep-breathing
maneuvers (at least every 2 hours) assist in preventing and treating
atelectasis. The performance of these maneuvers requires a patient who is alert
and cooperative. Patient education and reinforcement are key to the success of
these interventions. The use of incentive spirometry or voluntary deep
breathing enhances lung expansion, decreases the potential for airway closure,
and may generate a cough. Secretion management techniques may include directed
cough, suctioning, aerosol neb-ulizer treatments followed by chest physical
therapy (postural drainage and chest percussion), or bronchoscopy. In some
set-tings, a metered-dose inhaler (MDI) is used to dispense a bron-chodilator rather
than an aerosol nebulizer treatment. Chart 23-1 summarizes measures to prevent
atelectasis.
Management
The
goal in treating the patient with atelectasis is to improve ven-tilation and
remove secretions. The strategies to prevent atelec-tasis, which include
frequent turning, early ambulation, lung volume expansion maneuvers (eg,
deep-breathing exercises, in-centive spirometry), and coughing also serve as
the first-line mea-sures to minimize or treat atelectasis by improving
ventilation. In patients who do not respond to first-line measures or who
cannot perform deep-breathing exercises, other treatments such as posi-tive
expiratory pressure or PEP therapy (a simple mask and one-way valve system that
provides varying amounts of expiratory resistance [usually 5 to 15 cm H2O]),
continuous or intermittent positive pressure-breathing (IPPB), or bronchoscopy
may be used. Although IPPB may be used in some settings, few data sup-port its
use in the postoperative setting (Duffy & Farley, 1993). Before initiating
more complex, costly, and labor-intensive ther-apies, the nurse should ask
several questions:
· Has the patient been given an adequate trial of deep-breathing exercises?
·
Has the patient received adequate
education, supervision, and coaching to carry out the deep-breathing exercises?
·
Have other factors been evaluated
that may impair ventila-tion or prohibit a good patient effort (eg, lack of
turning, mobilization; excessive pain; excessive sedation)?
If
the cause of atelectasis is bronchial obstruction from secre-tions, the
secretions must be removed by coughing or suctioning to permit air to re-enter
that portion of the lung. Chest physical ther-apy (chest percussion and
postural drainage) may also be used to mobilize secretions. Nebulizer
treatments with a bronchodilator medication or sodium bicarbonate may be used
to assist the patient in the expectoration of secretions. If respiratory care
measures fail to remove the obstruction, a bronchoscopy is performed. Severe or
massive atelectasis may lead to acute respiratory failure, especially in a
patient with underlying lung disease. Endotracheal intubation and mechanical
ventilation may be necessary. Prompt treatment re-duces the risk for acute
respiratory failure or pneumonia.
If
atelectasis has resulted from compression of lung tissue, the goal is to
decrease the compression. With a large pleural effusion that is compressing
lung tissue and causing alveolar collapse, treatment may include thoracentesis, removal of the fluid by
needle aspiration, or insertion of a chest tube. The measures to increase lung
expansion described above also are used.
Management
of chronic atelectasis focuses on removing the cause of the obstruction of the
airways or the compression of the lung tissue. For example, bronchoscopy may be
used to open an airway obstructed by lung cancer or a nonmalignant lesion, and
the procedure may involve cryotherapy or laser therapy. The goal is to reopen
the airways and provide ventilation to the collapsed area. In some cases,
surgical management may be indicated.
Related Topics