Chapter: Medical Surgical Nursing: Management of Patients With Chest and Lower Respiratory Tract Disorders
Acute Respiratory Distress Syndrome
Acute Respiratory Distress Syndrome
Acute respiratory distress syndrome (ARDS;
previously calledadult respiratory distress syndrome) is a clinical syndrome
char-acterized by a sudden and progressive pulmonary edema, in-creasing
bilateral infiltrates on chest x-ray, hypoxemia refractory to oxygen
supplementation, and reduced lung compliance. These signs occur in the absence
of left-sided heart failure. Patients with ARDS usually require mechanical
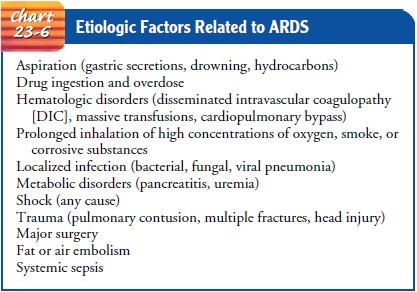
ventilation with a higher-than-normal airway pressure. A wide range of factors
are associated with the development of ARDS (Chart 23-6), including direct
injury to the lungs (eg, smoke inhalation) or indirect insult to the lungs (eg,
shock). ARDS has been associated with a mortality rate as high as 50% to 60%.
The major cause of death in ARDS is nonpulmonary multiple-system organ failure,
often with sepsis.
Pathophysiology
ARDS
occurs as a result of an inflammatory trigger that initiates the release of
cellular and chemical mediators, causing injury to the alveolar capillary
membrane. This results in leakage of fluid into the alveolar interstitial
spaces and alterations in the capillary bed.
Severe
ventilation–perfusion mismatching occurs in ARDS. Alveoli collapse because of
the inflammatory infiltrate, blood, fluid, and surfactant dysfunction. Small
airways are narrowed be-cause of interstitial fluid and bronchial obstruction.
The lung com-pliance becomes markedly decreased (stiff lungs), and the result
is a characteristic decrease in functional residual capacity and severe
hypoxemia. The blood returning to the lung for gas exchange is pumped through
the nonventilated, nonfunctioning areas of the lung, causing a shunt to
develop. This means that blood is inter-facing with nonfunctioning alveoli and
gas exchange is markedly impaired, resulting in severe, refractory hypoxemia.
Figure 23-6 shows the sequence of pathophysiologic events leading to ARDS.
Clinical Manifestations
Clinically,
the acute phase of ARDS is marked by a rapid onset of severe dyspnea that
usually occurs 12 to 48 hours after the ini-tiating event. A characteristic
feature is arterial hypoxemia that does not respond to supplemental oxygen. On
chest x-ray, the findings are similar to those seen with cardiogenic pulmonary
edema and present as bilateral infiltrates that quickly worsen. The acute lung
injury then progresses to fibrosing alveolitis with per-sistent, severe
hypoxemia. The patient also has increased alveolar dead space (ventilation to
alveoli, but poor perfusion) and de-creased pulmonary compliance (“stiff
lungs,” which are difficult to ventilate). Clinically, a patient is thought to
be in the recovery phase if the hypoxemia gradually resolves, the chest x-ray
im-proves, and the lungs become more compliant (Ware & Matthay, 2000).
Assessment and Diagnostic Findings
Intercostal retractions and crackles, as the fluid begins to leak into the alveolar interstitial space, are evident on physical examination. A diagnosis of ARDS may be made based on the following criteria: a history of systemic or pulmonary risk factors, acute onset of respiratory distress, bilateral pulmonary infiltrates, clinical absence of left-sided heart failure, and a ratio of partial pressure of oxygen of arterial blood to fraction of inspired oxygen (PaO2/FiO2) less than 200 mm Hg (severe refractory hypoxemia).
Medical Management
The
primary focus in the management of ARDS includes identi-fication and treatment
of the underlying condition. Aggressive, supportive care must be provided to
compensate for the severe respiratory dysfunction. This supportive therapy
almost always includes intubation and mechanical ventilation. In addition,
circulatory support, adequate fluid volume, and nutritional support are
important. Supplemental oxygen is used as the pa-tient begins the initial
spiral of hypoxemia. As the hypoxemia progresses, intubation and mechanical
ventilation are insti-tuted. The concentration of oxygen and ventilator
settings and modes are determined by the patient’s status. This is monitored by
arterial blood gas analysis, pulse oximetry, and bedside pul-monary function
testing.
Positive
end-expiratory pressure (PEEP) is a critical part of the treatment of ARDS.
PEEP usually improves oxygenation, but it does not influence the natural
history of the syndrome. Use of PEEP helps to increase functional residual
capacity and reverse alveolar collapse by keeping the alveoli open, resulting
in im-proved arterial oxygenation and a reduction in the severity of the
ventilation–perfusion imbalance. By using PEEP, a lower FiO2
may be required. The goal is a PaO2
greater than 60 mm Hg or an oxygen saturation level of greater than 90% at the
lowest pos-sible FiO2.
Systemic
hypotension may occur in ARDS as a result of hypovolemia secondary to leakage
of fluid into the interstitial spaces and depressed cardiac output from high
levels of PEEP therapy. Hypovolemia must be carefully treated without causing
further overload. Intravenous crystalloid solutions are adminis-tered, with
careful monitoring of pulmonary status. Inotropic or vasopressor agents may be
required. Pulmonary artery pressure catheters are used to monitor the patient’s
fluid status and the severe and progressive pulmonary hypertension sometimes
ob-served in ARDS.
PHARMACOLOGIC THERAPY
Numerous
pharmacologic treatments are under investigation to stop the cascade of events
leading to ARDS. These include human recombinant interleukin-1 receptor
antagonist, neu-trophil inhibitors, pulmonary-specific vasodilators, surfactant
re-placement therapy, antisepsis agents, antioxidant therapy, and
corticosteroids late in the course of ARDS (Ware & Matthay, 2000).
NUTRITIONAL THERAPY
Adequate
nutritional support is vital in the treatment of ARDS. Patients with ARDS
require 35 to 45 kcal/kg per day to meet caloric requirements. Enteral feeding
is the first consideration; however, parenteral nutrition also may be required.
Nursing Management
GENERAL MEASURES
The
patient with ARDS is critically ill and requires close moni-toring because the
condition could quickly change to a life-threatening situation.
In
addition to implementing the medical plan of care, the nurse considers other
needs of the patient. Positioning is impor-tant. The nurse should turn the
patient frequently to improve ventilation and perfusion in the lungs and
enhance secretion drainage. However, the nurse must closely monitor the patient
for deterioration in oxygenation with changes in position. Oxy-genation in the
ARDS patient is sometimes improved in the prone position and may be used in
special circumstances; studies to assess the benefits and problems of such
positioning are ongo-ing (Curley, 2000; Marion, 2001).
The
patient is extremely anxious and agitated because of the increasing hypoxemia
and dyspnea. The nurse should explain all procedures and provide care in a
calm, reassuring manner. It is important to reduce the patient’s anxiety
because anxiety pre-vents rest and increases oxygen expenditure. Rest is
essential to reduce oxygen consumption, thereby reducing oxygen needs.
VENTILATOR CONSIDERATIONS
If
the patient is intubated and receiving mechanical ventilation with PEEP,
several considerations must be addressed. PEEP, which causes increased
end-expiratory pressure, is an unnatural pattern of breathing and feels strange
to the patient. The patient may be anxious and “fight” the ventilator. Nursing
assessment is important to assess for problems with ventilation that may be
causing the anxiety reaction: tube blockage by kinking or retained secretions;
other acute respiratory problems (eg, pneumothorax, pain); a sudden drop in the
oxygen level; the patient’s level of dys-pnea; or ventilator malfunction. In
some cases, sedation may be required to decrease the patient’s oxygen consumption,
allow the ventilator to provide full support of ventilation, and decrease the
patient’s anxiety. Possible sedatives are lorazepam (Ativan), midazolam
(Versed), haloperidol (Haldol), propofol (Diprivan), and short-acting
barbiturates.
If
the PEEP level cannot be maintained despite the use of sedatives, neuromuscular
blocking agents, such as pancuronium (Pavulon), vecuronium (Norcuron),
atracurium (Tracrium), and rocuronium (Zemuron), may be given to paralyze the
patient. This allows the patient to be ventilated more easily. With paral-ysis,
the patient appears unconscious, loses motor function, and cannot breathe,
talk, or blink independently. However, the pa-tient retains sensation and is
awake and able to hear. The nurse must reassure the patient that the paralysis
is a result of the med-ication and is temporary. Paralysis should be used for
the short-est possible time and never without adequate sedation.
Use
of paralytic agents has many dangers and side effects. The nurse must be sure
the patient does not become disconnected from the ventilator, because
respiratory muscles are paralyzed and the patient will be apneic. Consequently,
the nurse ensures that the patient is closely monitored at all times. All
ventilator and pa-tient alarms should be on at all times. Eye care is important
as well because the patient cannot blink, increasing the risk of corneal
abrasions. Neuromuscular blockers predispose patients to the de-velopment of
deep venous thrombi, muscle atrophy, and skin breakdown. Nursing assessment is
essential to minimize the com-plications related to neuromuscular blockade. The
patient may have discomfort or pain but cannot communicate these
sensations.Analgesia is usually administered concurrently with neuromus-cular
blocking agents. The nurse must anticipate the patient’s needs regarding pain
and comfort. The nurse checks the patient’s position to ensure it is
comfortable and in normal alignment and talks to, and not about, the patient
while in the patient’s presence.
In
addition, it is important for the nurse to describe the pur-pose and effects of
the paralytic agents to the family. This expe-rience can be very frightening to
family members if they are unaware that these agents have been administered.
Related Topics